COMT Val158 Met基因多態(tài)性與恢復(fù)期晚發(fā)性抑郁癥患者腦白質(zhì)容積的關(guān)系
朱建英+++邵永良++任列++沈鑫華
[摘要] 目的 探討恢復(fù)期晚發(fā)性抑郁癥(RLOD)患者兒茶酚胺氧位甲基轉(zhuǎn)移酶(COMT)Val158 Met基因多態(tài)性與腦區(qū)體積、認(rèn)知功能的關(guān)系。 方法 選擇2014年5月~2015年5月湖州市第三人民醫(yī)院收治的符合DSM-Ⅳ重性抑郁障礙診斷標(biāo)準(zhǔn)的RLOD患者32例,按照COMT基因類型,分為Val純合子等位基因攜帶者(16例)和Met等位基因攜帶者(16例),分別檢測認(rèn)知功能頭顱MRI檢查。分析人口學(xué)資料、HDRS分值和神經(jīng)心理學(xué)測試進(jìn)行比較;以由中科院自動化研究所研發(fā)的半自動影像分析程序計算平均容積值;對攜帶有Met RLOD者體素集合的平均容積和神經(jīng)心理學(xué)測試結(jié)果進(jìn)行相關(guān)分析。 結(jié)果 Val純合子攜帶者和Met攜帶者間的數(shù)字廣度測試的比較差異有統(tǒng)計學(xué)意義(P < 0.05);相對攜帶Val純合子基因的RLOD患者,攜帶Met基因者的左楔前葉腦白質(zhì)顯著縮小(P < 0.001,未校正,體素值>100);攜帶Met的RLOD者,其楔前葉腦白質(zhì)容積同所有神經(jīng)心理學(xué)測試結(jié)果間無明顯相關(guān)性(P > 0.05)。 結(jié)論 COMT Val158 Met基因多態(tài)性與RLOD患者左楔前葉腦白質(zhì)容積異常存在關(guān)聯(lián)。
[關(guān)鍵詞] 兒茶酚胺氧位甲基轉(zhuǎn)移酶;基因多態(tài)性;恢復(fù)期晚發(fā)性抑郁癥;白質(zhì);認(rèn)知功能
[中圖分類號] R971.43 [文獻(xiàn)標(biāo)識碼] A [文章編號] 1673-7210(2017)04(b)-0124-04
[Abstract] Objective To explore the relationships between COMT Val158 Met gene polymorphism in patients with remitted late-onset depression (RLOD), volume of the encephalic regions and cognitive functions. Methods From May 2014 to May 2015, in Third Hospital of Huzhou, 32 RLOD patients who met the DSM-Ⅳ criteria for major depressive disorder wre selected. The patients were divided into two groups: 16 patients with Val homozygotes allele carriers and 16 patients with Met carriers according to COMT genotyping of the RLOD patients, and all subjects received the cognitive function test with the neuropsychological battery and the whole brain MRI scan; demographic data, HDRS scores, neural psychology test results were analyzed, a semiautomatic image analysis program developed by Chinese Academy of Sciences Institute of automation were applied to calculate the average volume of brain. Relationships between the average volume of Met allele carriers in RLOD patients and neural psychology test results were evaluated. Results There was significant difference in Digit Span Test between Val homozygotes and Met carriers (P < 0.05). The white matter volume of left precuneus in RLOD patients with Met carriers was significantly smaller than those with Val homozygotes (P < 0.001, uncorrected, voxel > 100). There were no significant correlations between the white matter volume of the left precuneus and all neuropsychological tests in RLOD patients with Met carriers (P > 0.05). Conclusion COMT Val158 Met gene polymorphism is associated with the white matter volume abnormality of left precuneus in the LOD patients.
[Key words] Catechol-o-methyltransferase; Gene polymorphism; Remitted late-onset depression ; White matter ; Cognitive function
晚發(fā)性抑郁癥患者存在認(rèn)知損害[1]。Pisljar等[2]發(fā)現(xiàn),恢復(fù)期晚發(fā)性抑郁癥(remitted late-onset depression,RLOD)患者的Stroop詞色測驗的絕對反應(yīng)時間顯著高于正常對照組。Lim等[3]報告晚發(fā)性抑郁癥(Late-onset depression,LOD)患者記憶功能和中顳葉、扣帶回峽部、楔前葉皮層厚度相關(guān);Hahn等[4]認(rèn)為未用藥晚發(fā)性抑郁癥患者前后胼胝體的體積較正常對照組小,后胼胝體體積和單詞清單記憶,單詞清單再認(rèn),結(jié)構(gòu)行為得分正相關(guān)。Tekin等[5]認(rèn)為額葉-皮質(zhì)下神經(jīng)環(huán)路障礙可能是抑郁癥認(rèn)知功能損害的基礎(chǔ);Dalby等[6]發(fā)現(xiàn)LOD患者左側(cè)上縱索、右側(cè)胼胝體向前額葉投射的白質(zhì)纖維束損傷更嚴(yán)重,影響認(rèn)知和情緒。可見,LOD的認(rèn)知損害可能存在腦結(jié)構(gòu)影像學(xué)方面的改變。有研究認(rèn)為COMT 158val/val基因型和早發(fā)性抑郁癥存在關(guān)聯(lián)[7],但也有認(rèn)為和抑郁癥無關(guān)聯(lián)[8];與抗抑郁藥4~6周療效不佳關(guān)聯(lián)[9];Atake等[10]發(fā)現(xiàn)COMTval/val基因型抑郁癥患者用度洛西汀治療時去甲腎上腺素能神經(jīng)元影響更敏感。可以推測,RLOD患者認(rèn)知功能、腦結(jié)構(gòu)的改變、特定的基因型之間可能存在關(guān)聯(lián)。
1 資料與方法
1.1 一般資料
3選擇2014年5月~2015年5月湖州市第三人民醫(yī)院收治的符合DSM-Ⅳ重性抑郁障礙診斷標(biāo)準(zhǔn)的RLOD患者32例,其中男16例,女16例,平均年齡為(69.98±4.63)歲。所有患者均由2名資深且經(jīng)驗豐富的精神科醫(yī)師以半結(jié)構(gòu)式訪談的方式對其進(jìn)行訪談,內(nèi)容包括醫(yī)師版的DSM-Ⅳ軸Ⅰ障礙(SCID-Ⅰ)結(jié)構(gòu)式臨床訪談[11]。在所有32例患者中,服用舍曲林10例,平均劑量(85.00±24.15)mg/d;帕羅西汀12例,平均劑量(25.83±6.69)mg/d;文拉法辛10例,平均劑量(142.50±42.57)mg/d;所有受試者均為右利手且無表達(dá)障礙的漢族。根據(jù)COMT基因類型,ROLD患者共分為兩組,包括16例Val純合子等位基因攜帶者和16例Met等位基因攜帶者。本研究經(jīng)醫(yī)院醫(yī)學(xué)倫理委員會批準(zhǔn),在詳細(xì)解釋研究過程并做充分釋疑后,所有患者和/或家屬均知情同意并簽署知情同意書。
納入標(biāo)準(zhǔn):①入組前曾經(jīng)符合DSM-Ⅳ重癥抑郁障礙的診斷標(biāo)準(zhǔn),并緩解超過6個月;②首次發(fā)作,且發(fā)作年齡為60歲以上;③HDRS<7分,且MMSE>24分;④病程<5年,且評估前停藥≥3個月。
排除標(biāo)準(zhǔn):①合并其他精神疾病,如物質(zhì)濫用或戒斷等;②有原發(fā)性神經(jīng)疾病,如癡呆或腦卒中;③合并損害認(rèn)知功能的軀體疾病;④有電抽搐治療經(jīng)歷;⑤T2權(quán)重的MRI檢查有任何因梗塞灶或其他血管損傷等引發(fā)的明顯白質(zhì)變化。
1.2 方法
1.2.1 神經(jīng)心理學(xué)測驗 所有受試者均由前述兩名精神科醫(yī)師采用標(biāo)準(zhǔn)化方式對其進(jìn)行神經(jīng)心理學(xué)評估,包括簡易智力狀態(tài)檢查(MMSE)、Rey聽說學(xué)習(xí)測驗(RAVLT)、Rey-Osterrieth復(fù)合數(shù)字測試(CFT),連線測試A和B,數(shù)字廣度測驗,符號數(shù)字轉(zhuǎn)換測驗和畫鐘測驗。
1.2.2 COMT基因檢測 采用聚合酶鏈反應(yīng)-限制性片段長度的多態(tài)性方法檢測患者COMT val158 met突變點基因多態(tài)性。COM Tval158 met引物合成參考Daniels等[12]的文獻(xiàn)所述方法。
1.2.3 MRI資料獲取 General Electric 1.5 Tesla MRI儀對受試者實施檢測。以3D擾相梯度回波序列(SPGR)獲取全腦的高分辨T1權(quán)重軸影像:重復(fù)時間=9.9ms,回聲時間=2.1 ms;投射角度=15°,獲取矩陣=256×192;視野=240 mm×240 mm,厚度=2.0 mm,間隔=0 mm,激發(fā)次數(shù)=1.0。
1.2.4 影像數(shù)據(jù)分析 結(jié)構(gòu)性數(shù)據(jù)分析及萎縮測量采用基于體素形態(tài)學(xué)方法。所有解剖學(xué)數(shù)據(jù)均由VBM5工具箱以及SPM 5軟件包處理,工具箱兼用SPM 5的分割十進(jìn)制算法和隱馬爾科夫隨機領(lǐng)域的擴展法。對結(jié)構(gòu)性影像分析則采用VBM 5工具箱,在預(yù)處理期間,對灰質(zhì)影像進(jìn)行調(diào)整以補償空間常態(tài)化效應(yīng),之后采用基于體素的分析方法對Val純合子基因攜帶RLOD者和非攜帶者的灰質(zhì)容積進(jìn)行比較。在進(jìn)行腦容積局部改變的組間比較時,采用“two-sample test”,設(shè)定閾高為P < 0.001,閾寬>100 mm3(集合距=1 mm×1 mm×1 mm)。
1.3 統(tǒng)計學(xué)方法
采用SPSS 10.0統(tǒng)計軟件,以獨立樣本t檢驗和χ2對組間的人口學(xué)資料、HDRS分值和神經(jīng)心理學(xué)測試進(jìn)行比較,另外,本研究提取了組間顯示差異性RLOD者體素集合的平均容積,兩者分別攜帶有Val純合子和Met,以由中科院自動化研究所研發(fā)的半自動影像分析程序計算平均容積值,以Pearson相關(guān)對攜帶有Met RLOD者體素集合的平均容積和神經(jīng)心理學(xué)測試結(jié)果進(jìn)行相關(guān)分析。以P < 0.05為差異有統(tǒng)計學(xué)意義。
2 結(jié)果
2.1 人口學(xué)資料和神經(jīng)心理學(xué)特征
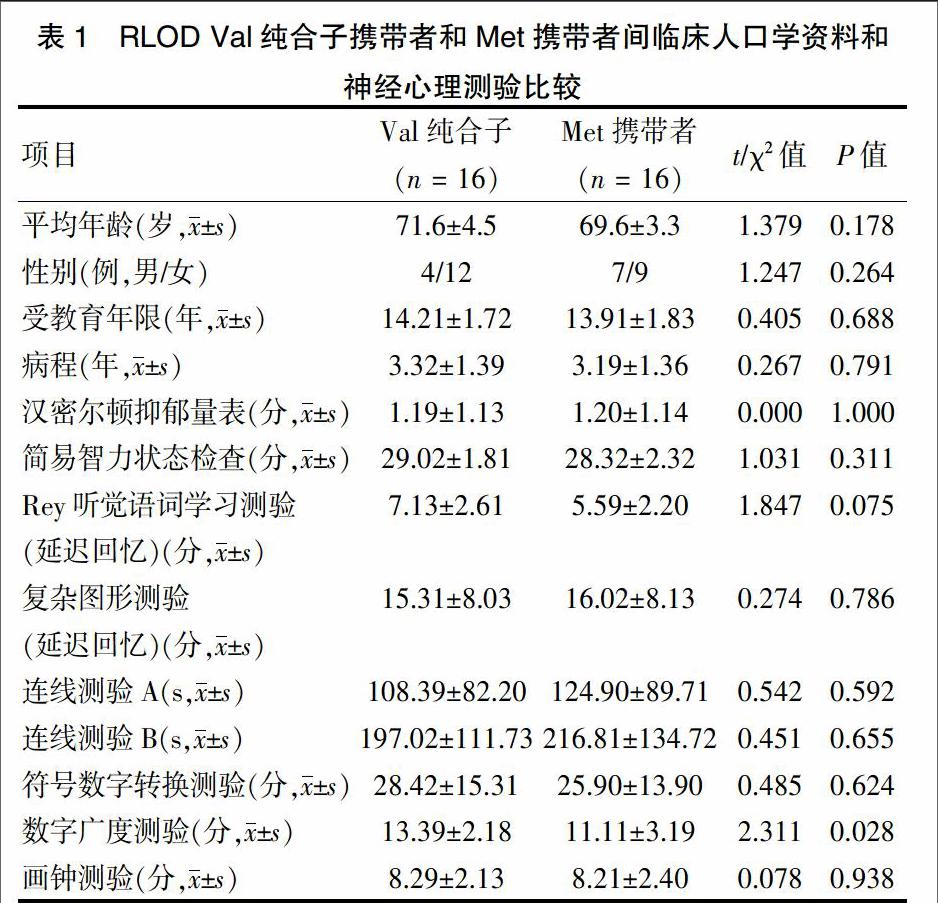
受試者人口學(xué)資料和神經(jīng)心理學(xué)特征詳見表1。Val純合子攜帶者和Met攜帶者間的數(shù)字廣度測試存在統(tǒng)計學(xué)意義差異(P < 0.05),而兩組間在年齡、性別分布、受教育年限,HDRS分值及其他神經(jīng)心理學(xué)測試結(jié)果方面差異無統(tǒng)計學(xué)意義(P > 0.05)。
2.2 左楔前葉腦白質(zhì)體積
相對攜帶Val純合子基因的RLOD者而言,攜帶Met基因者的左楔前葉腦白質(zhì)顯著縮小(Z值:5.76;MINI坐標(biāo):-8、-59、39,P < 0.001,未校正;體素值:1139)(圖1)。對攜帶Met的RLOD者而言,其楔前葉腦白質(zhì)容積同所有神經(jīng)心理學(xué)測試結(jié)果間無明顯相關(guān)性(r = -0.151~0.330,P = 0.213~0.967)。
3 討論
本研究發(fā)現(xiàn),COMTval純合子攜帶者和Met攜帶者間的數(shù)字廣度測試存在差異。進(jìn)一步證實了LOD存在認(rèn)知功能損害。Wang等[13]的研究認(rèn)為COMT val 158 met基因多態(tài)和認(rèn)知功能無關(guān)聯(lián)性,并且不能解釋抑郁癥患者認(rèn)知功能較非抑郁老人差的結(jié)果。
楔前葉皮層和皮層下聯(lián)接非常廣泛:頂葉側(cè)面中部、額葉、顳上溝、丘腦、紋狀體、屏狀核和腦干。功能影像學(xué)對正常人的研究提示,楔前葉在視覺空間成像功能、情景記憶提取功能和自我加工操作功能等方面起著重要作用[14]。Lim等[3]、Yin等的研究發(fā)現(xiàn)[15],抑郁癥患者存在楔前葉的結(jié)構(gòu)和功能異常。Gunning-Dixon等[16]也發(fā)現(xiàn),老年抑郁癥患者存在左側(cè)頂下小葉、楔前葉磁化傳遞率的下降,提示白質(zhì)纖維的結(jié)構(gòu)受損;Dalby等[17]發(fā)現(xiàn)LOD存在多個腦區(qū)深部白質(zhì)病變(DTI);Dalby等[6]報告LOD左側(cè)上縱索、右側(cè)胼胝體向前額葉投射的白質(zhì)纖維束損傷更嚴(yán)重,影響認(rèn)知和情緒。本研究發(fā)現(xiàn),相對攜帶Val純合子基因的ROLD患者,攜帶Met基因者的左楔前葉腦白質(zhì)顯著縮小。攜帶Met的晚發(fā)性抑郁癥患者,其楔前葉腦白質(zhì)容積同所有神經(jīng)心理學(xué)測試結(jié)果間無明顯相關(guān)性。筆者推測,LOD楔前葉白質(zhì)容積和基因型存在關(guān)聯(lián)性。
COMT基因編碼的是兒茶酚胺氧位甲基轉(zhuǎn)移酶。兒茶酚胺氧位甲基轉(zhuǎn)移酶是兒茶酚胺(包括腎上腺素、去甲腎上腺素和多巴胺)的主要代謝酶。人類COMT基因在其第4號外顯子存在1個G與A的置換點突變,使其編碼的108/158位氨基酸由Val變成Met,導(dǎo)致COMT酶的3~4倍活性改變。當(dāng)其108/158位氨基酸為Met時,該酶的活性變?yōu)椴荒蜔幔词乖谏項l件下,其活性也大大降低。眾所周知,中樞去甲腎上腺素和多巴胺的水平和抑郁關(guān)系密切,所以COMT含量或活性異常可能導(dǎo)致抑郁癥狀[18]。此外,抑郁患者可能存在周圍血BDNF水平的降低[19-20],BDNF通過不同途徑調(diào)控神經(jīng)細(xì)胞的生存、生長、分化和凋亡,可能會使某些腦區(qū)體積縮小。
Kupfer等[21]認(rèn)為抑郁癥的情緒處理、調(diào)節(jié)系統(tǒng)包括犒賞系統(tǒng)(如杏仁核、腹側(cè)紋狀體);中部前額葉皮層和前扣帶回皮層與情緒的自動調(diào)節(jié)有關(guān);外側(cè)前額葉皮層系統(tǒng)(如腹外側(cè)前額葉皮層和背外側(cè)前額葉皮層)和認(rèn)知、情緒的自動調(diào)節(jié)有關(guān)。此外,抑郁癥患者對負(fù)性信息特別敏感,在fMRI研究中表現(xiàn)為杏仁核等部位活動亢進(jìn)。楔前葉皮層和情景記憶提取、自我加工操作功能有關(guān);且和額葉、紋狀體等情緒調(diào)節(jié)部位存在非常緊密的聯(lián)系,而不同腦區(qū)的連接,白質(zhì)起到了極期重要的作用,所以,有理由推測,抑郁癥患者楔前葉白質(zhì)容積異常可能和抑郁的發(fā)生存在關(guān)系。
白質(zhì)病變往往由小血管的退化所引起,高血壓和動脈硬化是重要的危險因素。故有學(xué)者[22]認(rèn)為,腦血管病也許比糖皮質(zhì)激素介導(dǎo)的腦損害在老年抑郁癥的持續(xù)認(rèn)知損害中更重要。這提示臨床醫(yī)師要重視LOD的白質(zhì)改變。更進(jìn)一步地,要重視可能導(dǎo)致白質(zhì)病變的小血管退化的相關(guān)因素。這樣拓展了LOD的預(yù)防、診斷、治療、康復(fù)思路。
本研究僅僅是橫斷面、非動態(tài)的研究,且樣本量少,所以結(jié)論僅僅是初步的。在晚發(fā)性抑郁癥的研究中,把認(rèn)知、結(jié)構(gòu)影像、基因多態(tài)結(jié)合起來可能是一個研究方向。
[參考文獻(xiàn)]
[1] Yin Y,Hou Z,Wang X,et al. Association between altered resting-state cortico-cerebellar functional connectivity networks and mood/cognition dysfunction in late-onset depression [J]. J Neural Transm (Vienna),2015,122(6):887-896.
[2] Pisljar M,Repovs G,Pirtosek Z. Cognition in late onset depression [J]. Psychiatry Res,2013,210(1):89-94.
[3] Lim HK,Jung WS,Ahn KJ,et al. Regional cortical thickness and subcortical volume changes are associated with cognitive impairments in the drug-naive patients with late-onset depression [J]. Neuropsychopharmacology,2012,37(3):838-849.
[4] Hahn C,Lim HK,Won WY,et al. Sub-regional volumes changes of the corpus callosum in the drug naive patients with late-onset depression [J]. Prog Neuropsychopharmacol Biol Psychiatry,2015,56:46-51.
[5] Tekin S,Cummings JL. Frontal-subcortical neuronal circuits and clinical neuropsychiatry:an update [J]. J Psychosom Res,2002,53(2):647-654.
[6] Dalby RB,Chakravarty MM,Ahdidan J,et al. Localization of white-matter lesions and effect of vascular risk factors in late-onset major depression [J]. Psychol Med,2010,40(8):1389-1399.
[7] Massat I,Souery D,Del-Favero J,et al. Association between COMT (Val158Met) functional polymorphism and early onset in patients with major depressive disorder in a European multicenter genetic association study [J]. Mol Psychiatry,2005,10(6):598-605.
[8] Klein M,Schmoeger M,Kasper S,et al. Meta-analysis of the COMT Val158Met polymorphism in major depressive disorder: the role of gender [J]. World J Biol Psychiatry,2016,17(2):147-58
[9] Baune BT,Hohoff C,Berger K,et al. Association of the COMT val158met variant with antidepressant treatment response in major depression [J]. Neuropsychopharmacology,2008,33(4):924-932.
[10] Atake K, Yoshimura R, Hori H,et al. Catechol-O-methyltransferase Val158Met genotype and the clinical responses to duloxetine treatment or plasma levels of 3-methoxy-4-hydroxyphenylglycol and homovanillic acid in Japanese patients with majordepressive disorder [J]. Neuropsychiatr Dis Treat,2015,11:967-974.
[11] First M B,Gibbon M. User's guide for the structured clinical interview for DSM-IV axis I disorders:SCID-1 clinician version [M]. American Psychiatric Pub:1997.
[12] Daniels JK,Williams NM,Williams J,et al. No evidence for allelic association between schizophrenia and a polymorphism determining high or low catechol O-methyltransferase activity [J]. Am J Psychiatry,1996,153(2):268-270.
[13] Wang X,Wang Z,Wu Y,et al. Association analysis of the catechol-O-methyltransferase /methylenetetrahydrofolate reductase genes andcognition in late-onset depression [J]. Psychiatry Clin Neurosci,2014,68(5):344-352.
[14] Cavanna AE,Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates [J]. Brain,2006,129(Pt 3):564-583.
[15] Yin Y,Hou Z,Wang X,et al. The BDNF Val66Met polymorphism,resting-state hippocampal functional connectivity and cognitive deficits in acute late-onset depression [J]. J Affect Disord,2015 ,183:22-30.
[16] Gunning-Dixon FM,Hoptman MJ,Lim KO,et al. Macromolecular white matter abnormalities in geriatric depression: a magnetization transfer imaging study [J]. Am J Geriatr Psychiatry,2008,16(4):255-262.
[17] Dalby RB,F(xiàn)randsen J,Chakravarty MM,et al. Correlations between Stroop task performance and white matter lesion measures in late-onset major depression [J]. Psychiatry Res,2012,202(2):142-149.
[18] Bremner JD,Vythilingam M,Ng CK,et al. Regional brain metabolic correlates of alpha-methylparatyrosine-induced depressive symptoms [J]. JAMA,2003,289(23):3125- 3134
[19] 沈鑫華,錢敏才,袁永貴,等.文拉法辛和帕羅西汀治療中重度抑郁癥的療效與血漿腦源性神經(jīng)營養(yǎng)因子水平變化的關(guān)系[J].中華精神科雜志,2011,44(3):190-191.
[20] Polyakova M,Stuke K,Schuemberg K,et al. BDNF as a biomarker for successful treatment of mood disorders: a systematic & quantitative meta-analysis [J]. J Affect Disord,2015,174:432-440.
[21] Kupfer DJ,F(xiàn)rank E,Phillips ML. Major depressive disorder:new clinical,neurobiological,and treatment perspectives [J]. Lancet,2012,379(9820):1045-1055.
[22] K■hler S,Thomas AJ,Lloyd A,et al. White matter hyperintensities,cortisol levels,brain atrophy and continuing cognitive deficits in late-life depression [J]. Br J Psychiatry,2010 ,196(2):143-149.
(收稿日期:2017-01-03 本文編輯:蘇 暢)

