初診雙相障礙Ⅱ型抑郁發(fā)作患者認(rèn)知功能改變及與臨床特征的關(guān)系研究
何琛琛 高媛 張明霞 劉燕霞 孫守強(qiáng)
摘要:目的? 探討初診雙相障礙Ⅱ型抑郁發(fā)作患者認(rèn)知功能改變及與臨床特征的關(guān)系。方法? 納入2018年1月-2021年1月我院就診初診雙相障礙Ⅱ型抑郁發(fā)作患者,以及同期招募的我院體檢中心完善檢查的健康人群各172例。比較兩組一般資料、臨床特征、精神分裂癥認(rèn)知功能評(píng)估成套測(cè)驗(yàn)認(rèn)知功能評(píng)分(MCCB)及認(rèn)知功能損傷發(fā)生率,并進(jìn)一步評(píng)價(jià)患者臨床癥狀與認(rèn)知功能間相關(guān)性。結(jié)果? 兩組性別、年齡及受教育年限比較,差異無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05);觀察組 HAMD24量表總分高于對(duì)照組(P<0.05);觀察組信息處理評(píng)分、注意力警覺(jué)評(píng)分、工作記憶評(píng)分、詞語(yǔ)學(xué)習(xí)評(píng)分、視覺(jué)學(xué)習(xí)評(píng)分、推理與問(wèn)題解決評(píng)分、社會(huì)認(rèn)知評(píng)分及MCCB量表總分低于對(duì)照組(P<0.05);觀察組低于1個(gè)、1.5個(gè)及2個(gè)標(biāo)準(zhǔn)差MCCB量表評(píng)分比例均高于對(duì)照組(P<0.05);相關(guān)性分析結(jié)果顯示,患者詞語(yǔ)學(xué)習(xí)能力、推理與問(wèn)題解決能力評(píng)分均與抑郁發(fā)作次數(shù)存在負(fù)相關(guān)關(guān)系(P<0.05);年齡、受教育年限、發(fā)作次數(shù)、總病程及HAMD24總分與MCCB量表評(píng)分間無(wú)相關(guān)性(P>0.05)。結(jié)論? 初診雙相障礙Ⅱ型抑郁發(fā)作患者認(rèn)知功能改變與抑郁發(fā)作次數(shù)密切相關(guān)。
關(guān)鍵詞:雙相情感障礙;抑郁發(fā)作;認(rèn)知功能;臨床特征
中圖分類(lèi)號(hào):R749.4? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? 文獻(xiàn)標(biāo)識(shí)碼:A? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? DOI:10.3969/j.issn.1006-1959.2024.11.013
文章編號(hào):1006-1959(2024)11-0074-05
Study on the Changes of Cognitive Function and its Relationship with Clinical Characteristics
in Patients with Newly Diagnosed Bipolar Disorder Type Ⅱ Depressive Episode
Abstract:Objective? To investigate the changes of cognitive function in patients with newly diagnosed bipolar disorder type Ⅱ depressive episode and its relationship with clinical characteristics.Methods? From January 2018 to January 2021, 172 patients with newly diagnosed bipolar disorder type Ⅱ depressive episode and 172 healthy people who were recruited in the physical examination center of our hospital during the same period were included. The general data, clinical characteristics, MATRICS Consensus Cognitive Battery(MCCB) and the incidence of cognitive impairment were compared between the two groups, and the correlation between clinical symptoms and cognitive function was further evaluated.Results? There was no significant difference in gender, age and years of education between the two groups (P>0.05). The total score of HAMD24 scale in the observation group was higher than that in the control group (P<0.05). The information processing score, attention alertness score, working memory score, word learning score, visual learning score, reasoning and problem solving score, social cognitive score and MCCB total score of the observation group were lower than those of the control group (P<0.05). The proportion of MCCB scale scores lower than 1, 1.5 and 2 standard deviations in the observation group was higher than that in the control group (P<0.05). The results of correlation analysis showed that the scores of patients' word learning ability, reasoning and problem solving ability were negatively correlated with the number of depressive episodes (P<0.05). There was no correlation between age, years of education, number of episodes, total course of disease and HAMD24 total score and MCCB scale score (P>0.05).Conclusion? The changes of cognitive function in patients with newly diagnosed bipolar disorder type Ⅱ depressive episode are closely related to the number of depressive episodes.
Key words:Bipolar disorder;Depressive episode;Cognitive function;Clinical characteristics
Ⅱ型雙相情感障礙患者主要臨床特征為心境不穩(wěn),存在躁狂、輕度躁狂發(fā)作或重度抑郁發(fā)作等癥狀[1];而認(rèn)知功能損傷被認(rèn)為是該病患者核心臨床癥狀,與情感癥狀獨(dú)立存在,故單純改善情緒癥狀往往難以有效促進(jìn)生活工作質(zhì)量恢復(fù),這一比例超過(guò)60%[2]。如何協(xié)助雙相情感障礙患者最大限度實(shí)現(xiàn)認(rèn)知痊愈越來(lái)越受到關(guān)注。但在臨床實(shí)踐過(guò)程中僅不足40%的雙相情感障礙患者檢測(cè)認(rèn)知功能,且情感障礙患者認(rèn)知損害癥狀評(píng)估缺乏統(tǒng)一標(biāo)準(zhǔn)[3]。有報(bào)道將認(rèn)知功能損傷定位為≥2個(gè)認(rèn)知領(lǐng)域得分下降1~2個(gè)標(biāo)準(zhǔn)差,但因納入人群和評(píng)定標(biāo)準(zhǔn)不統(tǒng)一導(dǎo)致研究結(jié)果存在較大差異[4]。基于以上證據(jù),本研究通過(guò)分析初診雙相障礙Ⅱ型抑郁發(fā)作患者認(rèn)知功能改變及與臨床特征的關(guān)系,旨在為后續(xù)認(rèn)知干預(yù)方案及個(gè)體化治療方案制定提供更多參考,現(xiàn)報(bào)道如下。
1資料與方法
1.1一般資料? 納入2018年1月-2021年1月于國(guó)藥東風(fēng)茅箭醫(yī)院/十堰市精神病醫(yī)院就診初診雙相障礙Ⅱ型抑郁發(fā)作患者(觀察組),另同期招募我院體檢中心完善檢查的健康人群(對(duì)照組),各172例。研究方案經(jīng)我院倫理委員會(huì)批準(zhǔn),研究對(duì)象知情同意并簽署同意書(shū)。
1.2納入與排除標(biāo)準(zhǔn)? 觀察組納入標(biāo)準(zhǔn):①由兩名中級(jí)及以上職稱(chēng)的高年資醫(yī)師評(píng)估符合DSM-5診斷標(biāo)準(zhǔn)[5];②首次診斷;③年齡18~60歲;④基線HAMD24評(píng)分≥20分,且基線YMRS評(píng)分<6分;⑤漢族;⑥右利手;⑦初中及以上文化水平。排除標(biāo)準(zhǔn):①合并其他精神系統(tǒng)疾病;②合并混合特征或其他類(lèi)型雙相情感障礙;③腦部器質(zhì)性疾病史或腦外傷史;④?chē)?yán)重軀體疾病;⑤酗酒或藥物濫用;⑥近6個(gè)月接受電休克治療;⑦妊娠或哺乳期女性。對(duì)照組納入標(biāo)準(zhǔn):①經(jīng)體檢證實(shí)身體健康;②基線HAMD24評(píng)分<8分,且基線YMRS評(píng)分<6分;③年齡18~60歲;④漢族;⑤右利手;⑥初中及以上文化水平。排除標(biāo)準(zhǔn):①精神系統(tǒng)疾病或家族史;②腦部器質(zhì)性疾病史或腦外傷史;③嚴(yán)重軀體疾病;④酗酒或藥物濫用;⑤妊娠或哺乳期女性。
1.3方法? 收集研究對(duì)象一般資料,包括年齡、性別、受教育時(shí)間、抑郁發(fā)作次數(shù)、病程及家族史。抑郁癥狀嚴(yán)重程度評(píng)估采用HAMD24量表,共24個(gè)條目,每個(gè)條目0~4分,分值越高提示抑郁癥狀越嚴(yán)重[6]。認(rèn)知功能評(píng)估采用MCCB量表,包括信息處理評(píng)分、注意力警覺(jué)評(píng)分、工作記憶評(píng)分、詞語(yǔ)學(xué)習(xí)評(píng)分、視覺(jué)學(xué)習(xí)評(píng)分、推理與問(wèn)題解決評(píng)分、社會(huì)認(rèn)知評(píng)分7部分,原始分?jǐn)?shù)經(jīng)中國(guó)常模轉(zhuǎn)換為T(mén)分計(jì)算總分[6]。認(rèn)知損傷發(fā)生判定標(biāo)準(zhǔn):以MCCB量表評(píng)分50分為均數(shù),10分為1個(gè)標(biāo)準(zhǔn)差,低于標(biāo)準(zhǔn)值1、1.5及2個(gè)標(biāo)準(zhǔn)差即可判定,MCCB評(píng)分包含7個(gè)維度共計(jì)10項(xiàng)條目,每項(xiàng)條目分值轉(zhuǎn)換后標(biāo)準(zhǔn)分之和即為MCCB總分(100分),總分越低代表認(rèn)知功能越差[6]。YMRS評(píng)分包括11個(gè)條目,其中第1、2、3、4、7、10、11個(gè)條目分值0~4分,其余條目分值0~8分,≥6分判定為存在躁狂癥狀,分值越高提示躁狂越嚴(yán)重。
1.4統(tǒng)計(jì)學(xué)方法? 采用SPSS 18.0軟件處理數(shù)據(jù),正態(tài)性評(píng)估采用Levene檢驗(yàn),其中符合正態(tài)分布計(jì)量資料比較采用t檢驗(yàn),以(x±s)表示。計(jì)數(shù)資料比較采用χ2檢驗(yàn)法,以[n(%)]表示;采用Spearman檢驗(yàn)評(píng)價(jià)臨床特征與認(rèn)知功能損傷間相關(guān)性,P<0.05為差異有統(tǒng)計(jì)學(xué)意義。
2結(jié)果
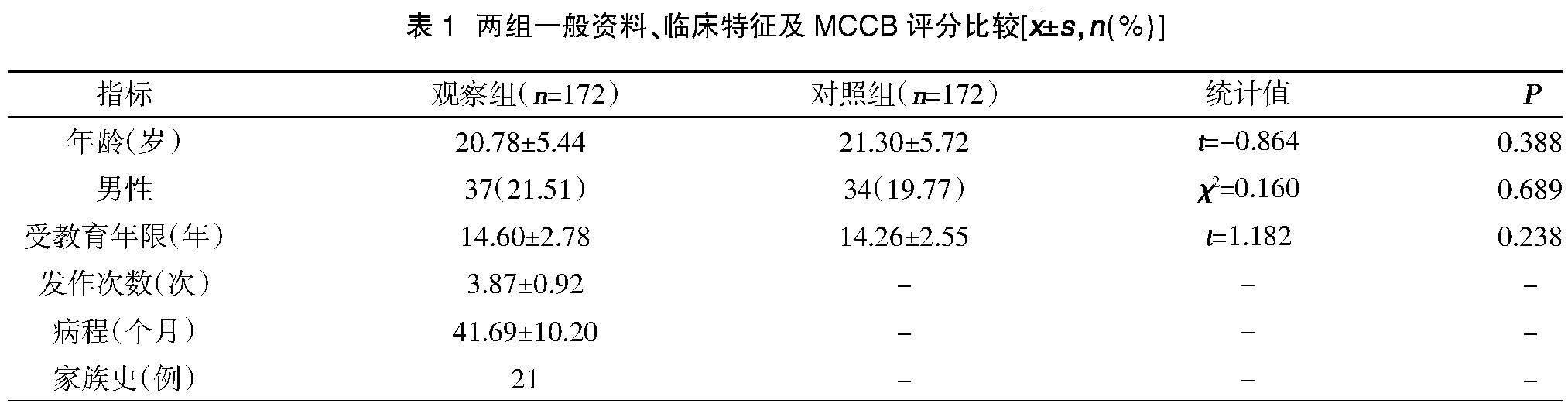
2.1兩組一般資料、臨床特征及MCCB評(píng)分比較? 兩組性別、年齡、受教育年限、YMRS評(píng)分比較,差異無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05);觀察組HAMD24量表總分高于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05);觀察組信息處理評(píng)分、注意力警覺(jué)評(píng)分、工作記憶評(píng)分、詞語(yǔ)學(xué)習(xí)評(píng)分、視覺(jué)學(xué)習(xí)評(píng)分、推理與問(wèn)題解決評(píng)分、社會(huì)認(rèn)知評(píng)分及MCCB量表總分低于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05),見(jiàn)表1。
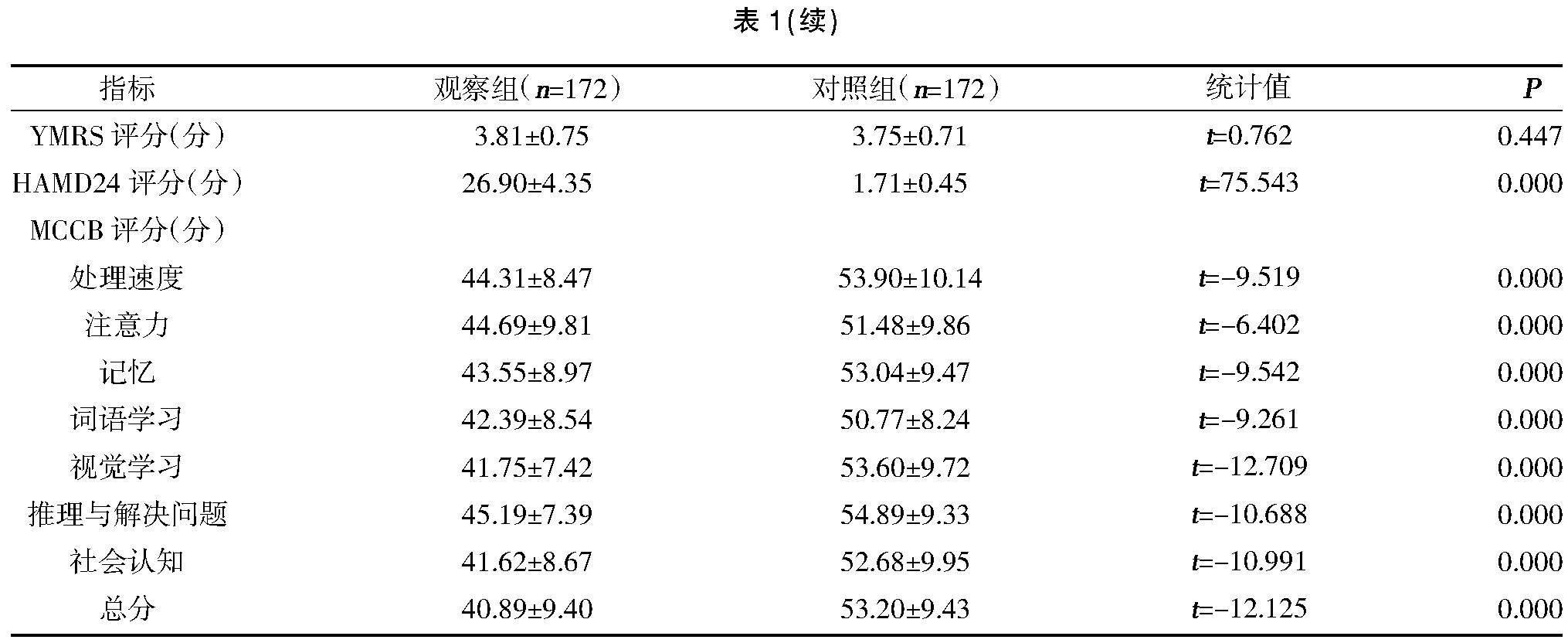
2.2兩組認(rèn)知功能損傷發(fā)生率比較? 觀察組低于1個(gè)、1.5個(gè)及2個(gè)標(biāo)準(zhǔn)差MCCB量表評(píng)分比例均高于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05),見(jiàn)表2。
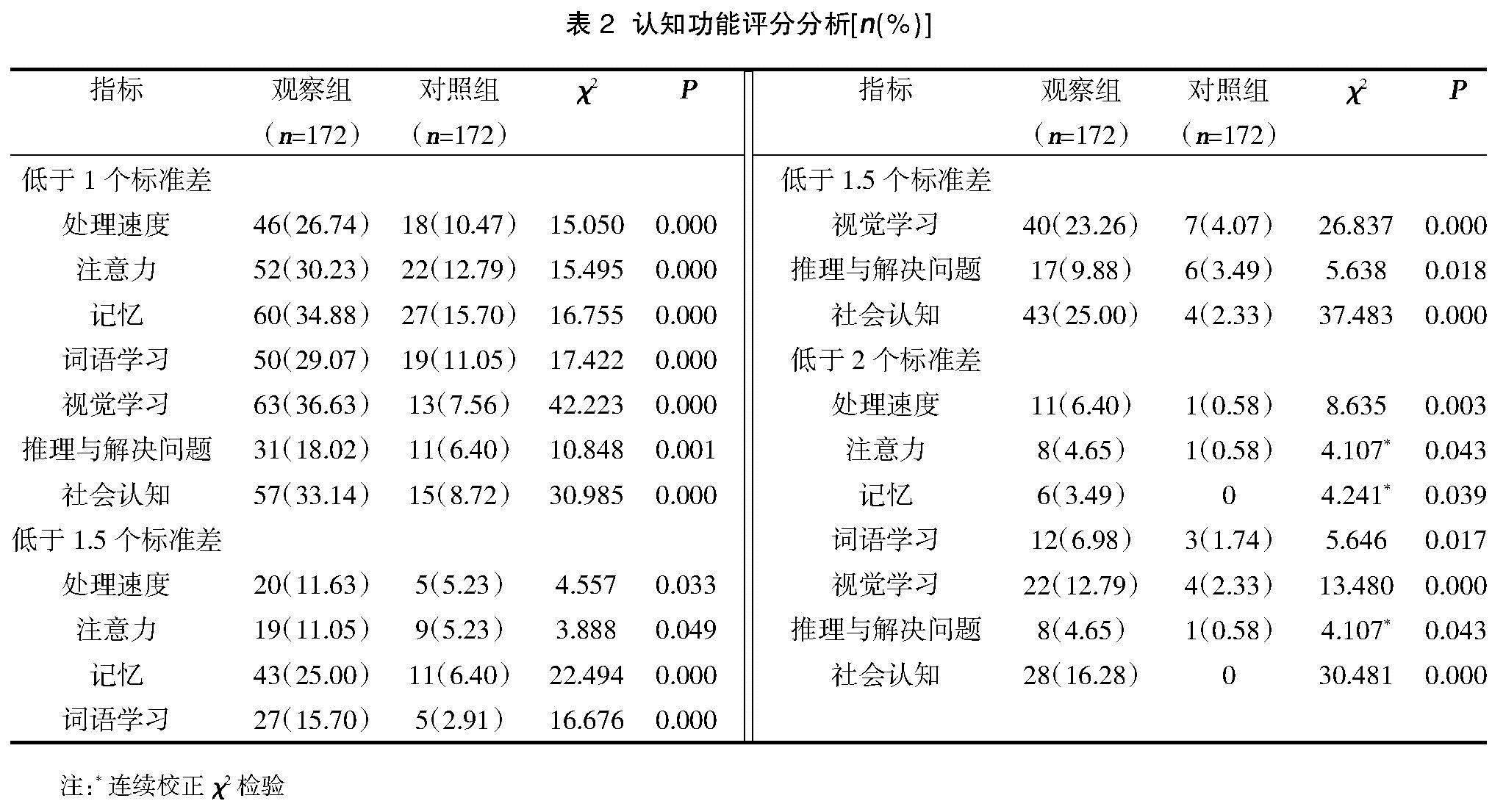
2.3患者臨床特征與MCCB評(píng)分間相關(guān)性分析? 相關(guān)性分析結(jié)果顯示,患者詞語(yǔ)學(xué)習(xí)能力、推理與問(wèn)題解決能力評(píng)分均與抑郁發(fā)作次數(shù)存在負(fù)相關(guān)關(guān)系(P<0.05);年齡、受教育年限、發(fā)作次數(shù)、總病程及HAMD24總分與MCCB量表評(píng)分間無(wú)相關(guān)性(P>0.05),見(jiàn)表3。
3討論
研究顯示[7,8],Ⅱ型雙相情感障礙患者往往伴有視覺(jué)、學(xué)習(xí)及記憶能力損傷等問(wèn)題,其中合并抑郁人群在視覺(jué)等信息處理方面障礙更為顯著,這可能與腦皮質(zhì)信息存儲(chǔ)、刷新及加工容量縮小有關(guān)。本次研究結(jié)果中,觀察組低于1個(gè)、1.5個(gè)及2個(gè)標(biāo)準(zhǔn)差MCCB量表評(píng)分比例均高于對(duì)照組(P<0.05),提示初診雙相障礙Ⅱ型抑郁發(fā)作患者在多個(gè)認(rèn)知領(lǐng)域均可見(jiàn)明顯損傷,與以往報(bào)道結(jié)果相符[9]。其中以<1.5個(gè)標(biāo)準(zhǔn)值作為認(rèn)知功能損傷判定標(biāo)準(zhǔn)時(shí),患者以記憶和社會(huì)認(rèn)知損傷最為常見(jiàn);而以<2個(gè)標(biāo)準(zhǔn)值作為判定標(biāo)準(zhǔn)時(shí),則損傷主要表現(xiàn)在視覺(jué)學(xué)習(xí)和社會(huì)認(rèn)知兩方面,進(jìn)一步證實(shí)此類(lèi)患者存在較為嚴(yán)重認(rèn)知領(lǐng)域損傷。臨床診療過(guò)程中相當(dāng)部分初診雙相障礙Ⅱ型抑郁發(fā)作患者盡管可觀察到明顯情緒癥狀緩解,但仍難以實(shí)現(xiàn)正常生活工作,造成這一現(xiàn)象可能原因即為潛在社會(huì)認(rèn)知功能異常[10]。
本次研究顯示,初診雙相障礙Ⅱ型抑郁發(fā)作患者M(jìn)CCB量表評(píng)分低于正常水平0.5~1.2個(gè)標(biāo)準(zhǔn)差,與以往研究報(bào)道結(jié)果基本相符[11]。將<1.5個(gè)標(biāo)準(zhǔn)值作為認(rèn)知功能損傷判定標(biāo)準(zhǔn)情況下,雙相情感障礙患者認(rèn)知功能損傷發(fā)生率為18%~42%,而體檢健康人群這一比例僅為2%,本次研究亦支持上述結(jié)果。而將<2個(gè)標(biāo)準(zhǔn)值作為認(rèn)知功能損傷判定標(biāo)準(zhǔn)情況下,有報(bào)道顯示35%雙相情感障礙患者存在≥2個(gè)認(rèn)知領(lǐng)域受損,而體檢健康人群這一比例僅為3%[12]。另一項(xiàng)研究中7%急性期雙相情感障礙患者存在認(rèn)知功能損傷,而緩解期這一比例達(dá)11%[13];采用這一標(biāo)準(zhǔn)本次研究納入初診雙相障礙Ⅱ型抑郁發(fā)作患者認(rèn)知功能損傷率達(dá)14%,而體檢健康人群無(wú)認(rèn)知功能損傷病例。本次研究納入患者認(rèn)知功能損傷比例與以往報(bào)道仍存在一定差異,這可能與以往研究中納入I型雙相情感障礙或Ⅱ型雙相情感障礙緩解期病例,且部分患者接受相應(yīng)治療有關(guān)[14]。此外,早期研究所采用認(rèn)知功能評(píng)估工具并不統(tǒng)一,多為單獨(dú)或幾個(gè)量表聯(lián)合[15],而本次研究采用MCCB量表評(píng)估更具臨床推廣應(yīng)用價(jià)值。
本次研究進(jìn)一步探討初診雙相障礙Ⅱ型抑郁發(fā)作患者臨床特征與認(rèn)知功能損傷間的相關(guān)性,最終結(jié)果顯示患者詞語(yǔ)學(xué)習(xí)能力、推理與問(wèn)題解決能力評(píng)分均與抑郁發(fā)作次數(shù)存在負(fù)相關(guān)關(guān)系(P<0.05);年齡、受教育年限、發(fā)作次數(shù)、總病程及HAMD24總分與MCCB量表評(píng)分間無(wú)相關(guān)性(P>0.05)。有報(bào)道顯示[16],無(wú)論躁狂發(fā)作抑或抑郁發(fā)作雙相情感障礙患者,發(fā)作次數(shù)越多則注意力和記憶力下降越明顯,同時(shí)躁狂發(fā)作次數(shù)與言語(yǔ)學(xué)習(xí)能力存在負(fù)相關(guān)關(guān)系。另有研究指出抑郁發(fā)作相較于躁狂或混合性發(fā)作次數(shù)與認(rèn)知功能缺損關(guān)系更為密切最密切,這可能與外周血中促炎細(xì)胞因子表達(dá)對(duì)于患者情緒癥狀發(fā)作及執(zhí)行功能損傷的影響有關(guān)[17]。
MCCB量表是現(xiàn)有較為全面認(rèn)知領(lǐng)域能力測(cè)評(píng)工具。但有報(bào)道顯示[18,19],MCCB評(píng)估推理與解決問(wèn)題分量表Cohen′s D=0.65,而WCST測(cè)驗(yàn)、Stroop 色詞測(cè)驗(yàn)或TMT-B測(cè)驗(yàn)相較于該分量表往往更加敏感,其中WSCT和TMT-B測(cè)驗(yàn)Cohen′s D分別達(dá)0.73,0.86。故后續(xù)研究除可選擇MCCB量表,更增加了聯(lián)合WCST、TMT-B等測(cè)驗(yàn)工具提高部分認(rèn)知功能損傷特征評(píng)估效能。
綜上所述,初診雙相障礙Ⅱ型抑郁發(fā)作患者認(rèn)知功能改變與抑郁發(fā)作次數(shù)密切相關(guān)。
參考文獻(xiàn):
[1]El Nagar Z,El Shahawi HH,Effat SM,et al.Single episode brief psychotic disorder versus bipolar disorder: A diffusion tensor imaging and executive functions study[J].Schizophr Res Cogn,2021,27(9):100214.
[2]Xu X,Xiang H,Qiu Y,et al.Sex differences in cognitive function of first-diagnosed and drug-naive patients with bipolar disorder[J].J Affect Disord,2021,295(9):431-437.
[3]Huang Y,Wang Y,Wang H,et al.Prevalence of mental disorders in China: a cross-sectional epidemiological study[J].Lancet Psychiatry,2019,6(3):211-224.
[4]Bomyea JA,Parrish EM,Paolillo EW,et al.Relationships between daily mood states and real-time cognitive performance in individuals with bipolar disorder and healthy comparators: A remote ambulatory assessment study[J].J Clin Exp Neuropsychol,2021,8(9):1-12.
[5]汪作為,馬燕桃,陳俊,等.中國(guó)雙相障礙防治指南:基于循證的選擇[J].中華精神科雜志,2017,50(2):96-100.
[6]Simjanoski M,McIntyre A,Kapczinski F,et al.Cognitive impairment in bipolar disorder in comparison to mild cognitive impairment and dementia: a systematic review[J].Trends Psychiatry Psychother,2021,9(8):1152-1159.
[7]Simjanoski M,Jansen K,Mondin TC,et al.Cognitive complaints in individuals recently diagnosed with bipolar disorder: A cross-sectional study[J].Psychiatry Res,2021,300(6):113894.
[8]Simonetti A,Kurian S,Saxena J,et al.Cognitive correlates of impulsive aggression in youth with pediatric bipolar disorder and bipolar offspring[J].J Affect Disord,2021,287(5):387-396.
[9]Douglas KM,Gallagher P,Robinson LJ,et al.Prevalence of cognitive impairment in major depression and bipolar disorder[J].Bipolar Disord,2018,20(3):260-274.
[10]Petersen JZ,Macoveanu J,Kj?rstad HL,et al.Assessment of the neuronal underpinnings of cognitive impairment in bipolar disorder with a picture encoding paradigm and methodological lessons learnt[J].J Psychopharmacol,2021,35(8):983-991.
[11]Miskowiak KW,Jespersen AE,Obenhausen K,et al.Internet-based cognitive assessment tool: Sensitivity and validity of a new online cognition screening tool for patients with bipolar disorder[J].J Affect Disord,2021,289(6):125-134.
[12]Liu T,Zhong S,Wang B,et al.Similar profiles of cognitive domain deficits between medication-na?ve patients with bipolar Ⅱ depression and those with major depressive disorder[J].J Affect Disord,2019,243(10):55-61.
[13]Ribera C,Vidal-Rubio SL,Romeu-Climent JE,et al.Cognitive impairment and consumption of mental healthcare resources in outpatients with bipolar disorder[J].J Psychiatr Res,2021,138(6):535-540.
[14]Callahan BL,McLaren-Gradinaru M,Burles F,et al.How Does Dementia Begin to Manifest in Bipolar Disorder? A Description of Prodromal Clinical and Cognitive Changes[J].J Alzheimers Dis,2021,82(2):737-748.
[15]Beunders AJM,Kemp T,Korten NCM,et al.Cognitive performance in older-age bipolar disorder: Investigating psychiatric characteristics, cardiovascular burden and psychotropic medication[J].Acta Psychiatr Scand,2021,144(4):392-406.
[16]Macoveanu J,F(xiàn)reeman KO,Kjaerstad HL,et al.Structural brain abnormalities associated with cognitive impairments in bipolar disorder[J].Acta Psychiatr Scand,2021,144(4):379-391.
[17]Burdick KE,Millett CE.Cognitive heterogeneity is a key predictor of differential functional outcome in patients with bipolar disorder[J].Eur Neuropsychopharmacol,2021,53(7):4-6.
[18]Millett CE,Harder J,Locascio JJ,et al.TNF-α and its soluble receptors mediate the relationship between prior severe mood episodes and cognitive dysfunction in euthymic bipolar disorder[J].Brain Behav Immun,2020,88(7):403-410.
[19]Tsapekos D,Strawbridge R,Cella M,et al.Cognitive impairment in euthymic patients with bipolar disorder: Prevalence estimation and model selection for predictors of cognitive performance[J].J Affect Disord,2021,294(11):497-504.
- 醫(yī)學(xué)信息的其它文章
- Modic源性下腰痛的病因?qū)W研究進(jìn)展
- 放射性口腔黏膜炎的評(píng)估、發(fā)病機(jī)制及預(yù)防研究
- 細(xì)節(jié)管理對(duì)小兒肺炎護(hù)理效果及患兒肺功能的影響
- 快速康復(fù)外科護(hù)理對(duì)剖宮產(chǎn)術(shù)后產(chǎn)婦早期離床活動(dòng)的影響
- 分階段延續(xù)護(hù)理干預(yù)對(duì)提高血液透析患者動(dòng)靜脈內(nèi)瘺自我護(hù)理能力的影響
- 雙向質(zhì)量反饋?zhàn)o(hù)理模式對(duì)肝硬化患者生活質(zhì)量與預(yù)后的影響

