多巴胺受體激動劑在治療不寧腿綜合征中的臨床應用
喻哲明金莉蓉(復旦大學附屬中山醫(yī)院神經內科 上海 200032)
多巴胺受體激動劑在治療不寧腿綜合征中的臨床應用
喻哲明*金莉蓉**
(復旦大學附屬中山醫(yī)院神經內科 上海 200032)
摘 要不寧腿綜合征主要表現(xiàn)為肢體感覺異常及難以控制的肢體活動,多在休息、睡眠時加重而在活動后緩解,患者還常伴有失眠等睡眠障礙。不寧腿綜合征的發(fā)生與多巴胺能系統(tǒng)異常密切相關,使用左旋多巴和多巴胺受體激動劑治療有效。其中,多巴胺受體激動劑是治療不寧腿綜合征的一線用藥,治療中、重度不寧腿綜合征的療效較好,患者的耐受性也佳,但長期使用時需注意患者癥狀加重、反跳等不良反應。
關鍵詞不寧腿綜合征 多巴胺受體激動劑 治療
Clinical application of dopaminergic agonists in the treatment of restless legs syndrome
YU Zheming*, JIN Lirong**
(Department of Neurology, Zhongshan Hospital, Fudan University, Shanghai 200032, China)
ABSTRACTRestless legs syndrome (RLS) is characterized by uncomfortable sensations and irresistible urges to move one’s legs, which is usually worse during the rest or sleep and can be relieved by movement. The pathophysiologic mechanism of RLS may be closely related to dopaminergic system and the use of levodopa and dopaminergic agonists for its treatment is effective, in which the first choice is dopaminergic agonists. Dopaminergic agonists are well tolerant in moderate and severe RLS, however, the adverse reactions such as augmentation and rebound should be taken into consideration in long-term treatment.
KEY WORDSrestless legs syndrome; dopaminergic agonists; treatment
不寧腿綜合征(restless legs syndrome, RLS)是一種與睡眠密切相關的感覺運動性疾病,主要表現(xiàn)為腿部或上肢深部的異常不適感覺。這種異常感覺常在休息、睡眠時加重,導致難以控制的肢體活動,但在身體活動后可得到緩解。
Thomas Willis最早于1672年以拉丁文描述了RLS的臨床表現(xiàn)。近年來,人們對RLS的病理生理機制有了更深入的認識,發(fā)現(xiàn)RLS的發(fā)病與多巴胺能系統(tǒng)異常密切相關。2003年Allen等[1]修訂的RLS診斷標準提出,RLS的相關臨床特征中包括“對多巴胺能藥物治療有反應”。多巴胺受體激動劑是RLS治療的一線用藥,本文就此相關內容作一概述。
1 RLS的發(fā)生率及臨床特征
RLS在不同國家或地區(qū)的發(fā)病率不同。在歐美國家人群中,7% ~ 10%的人會出現(xiàn)RLS的核心癥狀[2-4]。而在亞洲國家,RLS的發(fā)病率相對較低,其中在日本為4.6%[5],在中國臺灣地區(qū)成人中為1.57%[6],在上海地區(qū)50歲以上人群中為0.69%[7]。
1995年,國際RLS研究小組(The International Restless Legs Syndrome Study Group, IRLSSG)提出的RLS的核心臨床特征為:①由于腿部感覺異常導致腿部活動;②該癥狀在休息時出現(xiàn)或加重;③該癥狀會在身體活動后得到部分緩解;④該癥狀在傍晚或夜間加重[8]。只有同時滿足這4項特征才可被診斷為RLS。由于夜間異常的肢體活動,RLS患者還會出現(xiàn)睡眠障礙并因此產生日間思睡和疲倦等癥狀。嚴重的RLS患者甚至在白天也可出現(xiàn)難以控制的肢體活動。2003年,IRLSSG更新
了RLS診斷的基本條件、支持條件以及RLS相關的臨床特征(表1)[1],其中提到使用低劑量多巴胺能藥物可有效緩解RLS的臨床癥狀,并將此作為RLS診斷的支持條件之一。
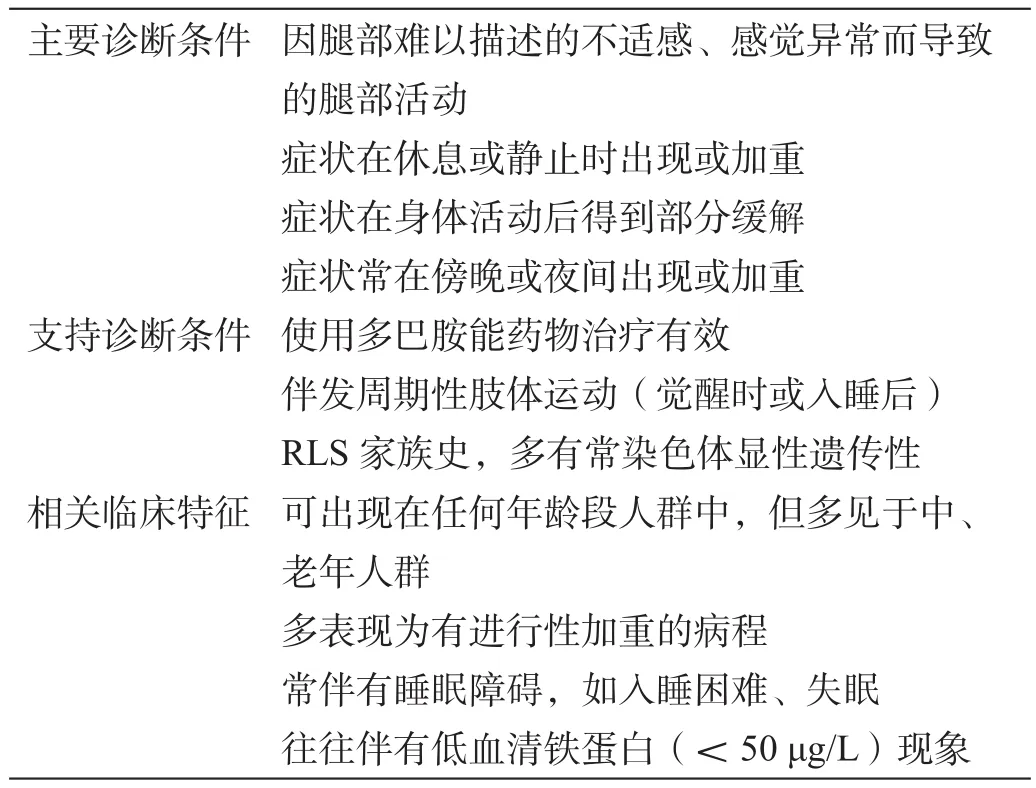
表1 RLS的診斷條件及相關臨床特征
臨床診斷RLS時還需與靜坐不能和神經根痛等疾病予于區(qū)分。有多種原因可導致靜坐不能。使用抗精神病藥物治療可出現(xiàn)靜坐不能[9],多表現(xiàn)為難以控制的全身活動,與嚴重RLS的表現(xiàn)類似,但活動后不會緩解。體位性低血壓患者久坐后也可能出現(xiàn)“難以控制的肢體活動”,多局限于下肢,且臥位或身體活動后能得到緩解,但一般沒有肢體深部的異常感覺。
神經根痛患者也會出現(xiàn)肢體深部的異常感覺,與RLS的表現(xiàn)類似,但還有在神經分布區(qū)域內的疼痛、麻木和肌肉萎縮等表現(xiàn)。此外,盡管部分患者在身體活動后可部分緩解異常的感覺癥狀,但并不會出現(xiàn)“難以控制的肢體活動”,且多巴胺能藥物治療無效。RLS還需與夜間腿部痙攣和下肢靜脈曲張等相區(qū)分,因這些疾病亦可導致患者出現(xiàn)夜間下肢異常感覺的表現(xiàn)。
2 RLS的治療藥物
RLS可分為原發(fā)性和繼發(fā)性兩類。目前,原發(fā)性RLS的具體發(fā)病機制不明,但有證據(jù)表明可能與多巴胺能系統(tǒng)障礙和鐵代謝異常密切相關[10]。A11細胞是脊髓內唯一一種多巴胺能神經元,被認為與RLS的發(fā)病密切相關[11]。通過刺激A11神經元可減少痛覺[12]。一些功能神經影像學如18F-多巴正電子發(fā)射斷層掃描術[13]、β-CIT單光子發(fā)射計算機斷層照像術[14-15]等研究結果也顯示,A11神經元的缺失及相關脊髓通路異常可部分解釋RLS的病理生理過程。鐵的缺乏會通過影響酪氨酸羥化酶而導致多巴胺合成減少。RLS的其他可能的發(fā)病機制還包括中樞神經系統(tǒng)神經遞質異常、遺傳因素、免疫功能障礙和炎癥機制等[10]。
繼發(fā)性RLS多繼發(fā)于其他疾病如尿毒癥、缺鐵性貧血、葉酸和維生素B12缺乏、干燥綜合征、帕金森病、小纖維神經病、多灶性神經病、腓骨肌萎縮癥、代謝病患者以及妊娠婦女中,使用三環(huán)類抗抑郁藥物、H2受體阻滯劑和鎮(zhèn)靜劑等也可能導致繼發(fā)性RLS[16]。發(fā)現(xiàn)并控制導致繼發(fā)性RLS的原因可部分緩解RLS的癥狀。對部分繼發(fā)性RLS患者,亦可給予用于原發(fā)性RLS的藥物治療。
RLS的主要治療目標是緩解癥狀、保持肢體正常功能和提高生活質量,現(xiàn)在臨床上使用的治療藥物包括多巴胺能藥物和非多巴胺能藥物。對間斷發(fā)作、每晚發(fā)作和難治性的RLS治療,美國RLS基金會醫(yī)學咨詢委員會(Medical Advisory Board of the Restless Legs Syndrome Foundation)已發(fā)表相關治療指南[17],其中肯定了多巴胺能藥物的臨床作用。
多巴胺能藥物包括左旋多巴和多巴胺受體激動劑。左旋多巴早就被用于治療輕度RLS。2009年中華醫(yī)學會發(fā)表的《不寧腿綜合征診斷標準和治療指南》[16]提出,對間歇發(fā)作的RLS患者,可以使用每日半片多巴絲肼或卡左雙多巴控釋片治療。每日使用左旋多巴會導致患者出現(xiàn)癥狀加重、反跳等不良反應。對每晚發(fā)作的RLS患者,推薦使用多巴胺受體激動劑治療[18],具體可選用普拉克索0.125 ~ 1.5 mg/d或羅匹尼羅0.5 ~ 6.0 mg/d。
多巴胺受體激動劑還可分為麥角類和非麥角類兩類。美國FDA批準治療RLS的非麥角類多巴胺受體激動劑有普拉克索、羅匹尼羅和羅替戈汀透皮貼膏[19-20],而培高利特等麥角類多巴胺受體激動劑因可導致心臟瓣膜損害等嚴重不良反應而未獲準治療RLS。已有多項隨機、對照試驗(randomized controlled trial, RCT)證實,非麥角類多巴胺受體激動劑治療RLS有效且耐受性和安全性均較好。
2.1 普拉克索
普拉克索通過刺激多巴胺D2和D3受體而產生多巴胺能效應。美國睡眠協(xié)會推薦使用普拉克索治療中、重度RLS(證據(jù)級別:高)[21],Garcia-Borreguero等[22]發(fā)表的歐洲RLS治療指南也指出普拉克索短期治療RLS有效、長期治療可能有效。多項短、長期研究結果均支
持普拉克索可有效降低中、重度RLS患者的《國際不寧腿量表》(International Restless Legs Scale, IRLS)評分[23-31]。一項對287例中國患者進行的持續(xù)6周的RCT結果顯示,普拉克索治療患者的IRLS評分下降幅度達73.8%(P<0.001),且《患者全面印象》(Patient Global Impression)評分改善幅度也達68.6%(P<0.001)[26]。在一項長期開放性試驗中,患者在基線、8和52周時的IRLS評分平均分別為22.3、11.1和4.9分,近86.6%的患者在52周時的IRLS評分下降幅度>50%[31]。薈萃分析表明,普拉克索治療可較安慰劑平均改善患者的IRLS評分5.96分(95% CI: 4.41 ~ 7.79分)[32]。
2.2 羅匹尼羅
羅匹尼羅是一種強效的多巴胺D2和D3受體激動劑,原被用于治療帕金森病,2005年又被歐美批準治療RLS。對5項短期RCT的薈萃分析顯示,羅匹尼羅治療可平均改善IRLS評分4分(95% CI: 2 ~ 6分)[21]。對基線IRLS評分>14分的RLS患者,一項26周的RCT及隨后40周的開放性研究結果均顯示,羅匹尼羅治療可較安慰劑顯著降低患者的IRLS評分[33]。此外,羅匹尼羅治療也可改善RLS患者的抑郁心境[34]和生活質量[35]等。
在普拉克索和羅匹尼羅的RCT中,RLS患者對普拉克索和羅匹尼羅治療的耐受性良好,報告較多(發(fā)生率>5%)的不良反應為惡心、頭痛、疲勞感、思睡、嘔吐、眩暈、失眠和鼻咽炎。目前尚未進行過直接比較普拉克索和羅匹尼羅治療RLS作用的RCT。但一項間接比較的薈萃分析顯示,普拉克索治療可較羅匹尼羅治療更顯著地降低IRLS評分和提高《臨床全面印象——全面改善》(Clinical Global Impression – Global Improvement, CGI-I)評分,同時較少發(fā)生惡心、嘔吐和眩暈等不良反應[36]。
2.3 羅替戈汀透皮貼膏
羅替戈汀透皮貼膏為選擇性的多巴胺D1、D2和D3受體激動劑,可經皮持續(xù)釋放藥物以維持穩(wěn)定的血藥濃度,已被批準用于治療RLS。2004年報告的一項為期1周的有63例中、重度RLS患者參加的RCT提示,羅替戈汀透皮貼膏治療能夠劑量依賴性地改善患者的癥狀,其中4.5 mg/d治療可顯著改善患者的IRLS評分(P<0.01)[37]。Oertel等[38]和Trenkwalder等[39]分別進行的為期6周和長達1年的RCT也顯示,羅替戈汀透皮貼膏3 mg/d治療中、重度RLS患者有效,但劑量更大(4 mg/d)卻無更大療效且不良反應更多。羅替戈汀透皮貼膏治療的常見不良反應主要包括頭痛和皮膚局部反應。近期完成的一項長達5年的開放性試驗結果顯示,早期RLS患者接受羅替戈汀透皮貼膏治療多會因皮膚局部反應等不良反應而終止治療,但羅替戈汀透皮貼膏對中、重度RLS患者有穩(wěn)定的療效(至少5年內)[40]。
2.4 吡貝地爾(piribedil)
吡貝地爾是選擇性多巴胺D2和D3受體激動劑,現(xiàn)尚未被批準用于RLS治療,但已有治療RLS有效和安全的研究報告。在一項臨床試驗中,17例RLS患者分別使用氯硝西泮或吡貝地爾治療4周,結果提示吡貝地爾治療組患者的癥狀改善程度更明顯(P<0.01),且不良反應僅為輕度胃腸道反應和心動過速,患者的依從性良好[41]。另一項為期10個月的開放性試驗顯示,吡貝地爾(25 ~ 100 mg/d)治療可改善RLS癥狀[42]。
3 RLS治療期間的注意事項
在使用多巴胺能藥物治療RLS期間可能出現(xiàn)癥狀惡化(augmentation)和反跳(rebound)等不良反應,這些不良反應更多見于長期、大量使用左旋多巴治療的患者,但在多巴胺受體激動劑治療RLS的研究中亦有類似報告。癥狀惡化包括5種情況:①與治療前相比,癥狀的嚴重程度加重;②休息時癥狀發(fā)生的潛伏期縮短;③白天發(fā)生癥狀;④癥狀從下肢發(fā)展至上肢、軀干;⑤藥效的持續(xù)時間縮短[43]。癥狀惡化的機制可能與中樞神經系統(tǒng)內多巴胺過量相關[44]。高濃度的多巴胺會使多巴胺D1受體興奮、引起多巴胺D1受體相關疼痛,從而產生周期性的肢體活動。使用小劑量多巴胺能藥物后出現(xiàn)癥狀加重的可能性較小。患者長期使用左旋多巴后出現(xiàn)癥狀惡化的比例在18% ~ 80%間[10]。普拉克索治療的癥狀惡化率為0% ~ 30%,但使用小劑量普拉克索時未見類似報告;羅匹尼羅治療的癥狀惡化率在4%左右[33,45]。RLS患者在出現(xiàn)輕度的癥狀加重后可在白天加用多巴胺能藥物,但一旦出現(xiàn)嚴重的癥狀加重時則需停用多巴胺能藥物而改用非多巴胺能藥物[46]。癥狀反跳多因為使用短效多巴胺能藥物所致,在藥效減退時出現(xiàn)RLS癥狀,又稱“劑末反跳”。RLS癥狀反跳多在凌晨出現(xiàn),此時可臨時加用1次短效多巴胺能藥物或改用長效多巴胺能藥物治療。
4 結語
除多巴胺能藥物外,抗驚厥藥物和阿片類藥物等治
療RLS也有一定的療效。一項薈萃分析提示,抗驚厥藥物如加巴噴丁等治療RLS的有效性已獲部分臨床試驗結果的支持,但仍需得到更多RCT的確認[47]。
參考文獻
[1] Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health [J]. Sleep Med, 2003, 4(2): 101-119.
[2] Berger K, Luedemann J, Trenkwalder C, et al. Sex and the risk of restless legs syndrome in the general population [J]. Arch Intern Med, 2004, 164(2): 196-202.
[3] Rothdach AJ, Trenkwalder C, Haberstock J, et al. Prevalence and risk factors of RLS in an elderly population: the MEMO study. Memory and Morbidity in Augsburg Elderly [J]. Neurology, 2000, 54(5): 1064-1068.
[4] Hogl B, Kiechl S, Willeit J, et al. Restless legs syndrome: a community-based study of prevalence, severity, and risk factors [J]. Neurology, 2005, 64(11): 1920-1924.
[5] Mizuno S, Miyaoka T, Inagaki T, et al. Prevalence of restless legs syndrome in non-institutionalized Japanese elderly [J]. Psychiatry Clin Neurosci, 2005, 59(4): 461-465.
[6] Chen NH, Chuang LP, Yang CT, et al. The prevalence of restless legs syndrome in Taiwanese adults [J]. Psychiatry Clin Neurosci, 2010, 64(2): 170-178.
[7] Ma JF, Xin XY, Liang L, et al. Restless legs syndrome in Chinese elderly people of an urban suburb in Shanghai: a community-based survey [J]. Parkinsonism Relat Disord, 2012, 18(3): 294-298.
[8] Walters AS. Toward a better definition of the restless legs syndrome. The International Restless Legs Syndrome Study Group [J]. Mov Disord, 1995, 10(5): 634-642.
[9] Agarkar S, Anthony D, Ferrando S. Risk of akathisia associated with atypical antipsychotics [J]. J Neuropsychiatry Clin Neurosci, 2013, 25(1): E46-E47.
[10] Nagandla K, De S. Restless legs syndrome: pathophysiology and modern management [J]. Postgrad Med J, 2013, 89(1053): 402-410.
[11] Ondo WG, He Y, Rajasekaran S, et al. Clinical correlates of 6-hydroxydopamine injections into A11 dopaminergic neurons in rats: a possible model for restless legs syndrome [J]. Mov Disord, 2000, 15(1): 154-158.
[12] Fleetwood-Walker SM, Hope PJ, Mitchell R. Antinociceptive actions of descending dopaminergic tracts on cat and rat dorsal horn somatosensory neurones [J]. J Physiol, 1988, 399: 335-348.
[13] Ruottinen HM, Partinen M, Hublin C, et al. An FDOPA PET study in patients with periodic limb movement disorder and restless legs syndrome [J]. Neurology, 2000, 54(2): 502-504.
[14] Linke R, Eisensehr I, Wetter TC, et al. Presynaptic dopaminergic function in patients with restless legs syndrome: are there common features with early Parkinson’s disease? [J]. Mov Disord, 2004, 19(10): 1158-1162.
[15] Eisensehr I, Wetter TC, Linke R, et al. Normal IPT and IBZM SPECT in drug-naive and levodopa-treated idiopathic restless legs syndrome [J]. Neurology, 2001, 57(7): 1307-1309.
[16] 中華醫(yī)學會神經病學分會帕金森病及運動障礙學組. 不寧腿綜合征的診斷標準和治療指南[J]. 中華神經科雜志, 2009, 42(10): 709-711.
[17] Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome [J]. Mayo Clin Proc, 2004, 79(7): 916-922.
[18] Trenkwalder C, Hening WA, Montagna P, et al. Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice [J]. Mov Disord, 2008, 23(16): 2267-2302.
[19] Bayard M, Avonda T, Wadzinski J. Restless legs syndrome [J]. Am Fam Physician, 2008, 78(2): 235-240.
[20] Stiasny K, Wetter TC, Trenkwalder C, et al. Restless legs syndrome and its treatment by dopamine agonists [J]. Parkinsonism Relat Disord, 2000, 7(1): 21-25.
[21] Aurora RN, Kristo DA, Bista SR, et al. The treatment of restless legs syndrome and periodic limb movement disorder in adults — an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses: an American Academy of Sleep Medicine Clinical Practice Guideline [J]. Sleep, 2012, 35(8): 1039-1062.
[22] Garcia-Borreguero D, Ferini-Strambi L, Kohnen R, et al. European guidelines on management of restless legs syndrome: report of a joint task force by the European Federation of Neurological Societies, the European Neurological Society and the European Sleep Research Society [J]. Eur J Neurol, 2012, 19(11): 1385-1396.
[23] Winkelman JW, Sethi KD, Kushida CA, et al. Efficacy and safety of pramipexole in restless legs syndrome [J]. Neurology, 2006, 67(6): 1034-1039.
[24] Partinen M, Hirvonen K, Jama L, et al. Efficacy and safety of pramipexole in idiopathic restless legs syndrome: a polysomnographic dose-finding study — the PRELUDE study [J]. Sleep Med, 2006, 7(5): 407-417.
[25] Oertel WH, Stiasny-Kolster K, Bergtholdt B, et al. Efficacy of pramipexole in restless legs syndrome: a six-week,
multicenter, randomized, double-blind study (effect-RLS study) [J]. Mov Disord, 2007, 22(2): 213-219.
[26] Ma JF, Wan Q, Hu XY, et al. Efficacy and safety of pramipexole in Chinese patients with restless legs syndrome: results from a multi-center, randomized, double-blind, placebo-controlled trial [J]. Sleep Med, 2012, 13(1): 58-63.
[27] Inoue Y, Kuroda K, Hirata K, et al. Efficacy, safety and dose-response of pramipexole in Japanese patients with primary restless legs syndrome: randomized trial [J]. Neuropsychobiology, 2011, 63(1): 35-42.
[28] Inoue Y, Hirata K, Kuroda K, et al. Efficacy and safety of pramipexole in Japanese patients with primary restless legs syndrome: a polysomnographic randomized, double-blind, placebo-controlled study [J]. Sleep Med, 2010, 11(1): 11-16.
[29] Ferini-Strambi L, Aarskog D, Partinen M, et al. Effect of pramipexole on RLS symptoms and sleep: a randomized, double-blind, placebo-controlled trial [J]. Sleep Med, 2008, 9(8): 874-881.
[30] Partinen M, Hirvonen K, Jama L, et al. Open-label study of the long-term efficacy and safety of pramipexole in patients with restless legs syndrome (extension of the PRELUDE study) [J]. Sleep Med, 2008, 9(5): 537-541.
[31] Inoue Y, Kuroda K, Hirata K, et al. Long-term open-label study of pramipexole in patients with primary restless legs syndrome [J]. J Neurol Sci, 2010, 294(1-2): 62-66.
[32] Zhang W, Wang Y, Cong SY, et al. Efficacy and tolerability of pramipexole for the treatment of primary restless leg syndrome: a meta-analysis of randomized placebo-controlled trials [J]. Neuropsychiatr Dis Treat, 2013, 9: 1035-1043.
[33] Giorgi L, Asgharian A, Hunter B. Ropinirole in patients with restless legs syndrome and baseline IRLS total scores ≥24: efficacy and tolerability in a 26-week, double-blind, parallelgroup, placebo-controlled study followed by a 40-week openlabel extension [J]. Clin Ther, 2013, 35(9): 1321-1336.
[34] Benes H, Mattern W, Peglau I, et al. Ropinirole improves depressive symptoms and restless legs syndrome severity in RLS patients: a multicentre, randomized, placebo-controlled study [J]. J Neurol, 2011, 258(6): 1046-1054.
[35] Cho YW, Hong SB, Kim do H, et al. The effect of ropinirole on the quality of life in patients with restless legs syndrome in Korea: an 8-week, multicenter, prospective study [J]. J Clin Neurol, 2013, 9(1): 51-56.
[36] Quilici S, Abrams KR, Nicolas A, et al. Meta-analysis of the efficacy and tolerability of pramipexole versus ropinirole in the treatment of restless legs syndrome [J]. Sleep Med, 2008, 9(7): 715-726.
[37] Stiasny-Kolster K, Kohnen R, Schollmayer E, et al. Patch application of the dopamine agonist rotigotine to patients with moderate to advanced stages of restless legs syndrome: a double-blind, placebo-controlled pilot study [J]. Mov Disord, 2004, 19(12): 1432-1438.
[38] Oertel WH, Benes H, Garcia-Borreguero D, et al. Efficacy of rotigotine transdermal system in severe restless legs syndrome: a randomized, double-blind, placebo-controlled, six-week dose-finding trial in Europe [J]. Sleep Med, 2008, 9(3): 228-239.
[39] Trenkwalder C, Benes H, Poewe W, et al. Efficacy of rotigotine for treatment of moderate-to-severe restless legs syndrome: a randomised, double-blind, placebo-controlled trial [J]. Lancet Neurol, 2008, 7(7): 595-604.
[40] Oertel W, Trenkwalder C, Benes H, et al. Long-term safety and efficacy of rotigotine transdermal patch for moderate-tosevere idiopathic restless legs syndrome: a 5-year open-label extension study [J]. Lancet Neurol, 2011, 10(8): 710-720.
[41] 江紅, 鄭凱, 史庭慧. 吡貝地爾治療不寧腿綜合征的臨床研究[J]. 卒中與神經疾病, 2006, 13(6): 363-365.
[42] Evidente VG. Piribedil for restless legs syndrome: a pilot study [J]. Mov Disord, 2001, 16(3): 579-581.
[43] Vetrugno R, Contin M, Baruzzi A, et al. Polysomnographic and pharmacokinetic findings in levodopa-induced augmentation of restless legs syndrome [J]. Mov Disord, 2006, 21(2): 254-258.
[44] Paulus W, Trenkwalder C. Less is more: pathophysiology of dopaminergic-therapy-related augmentation in restless legs syndrome [J]. Lancet Neurol, 2006, 5(10): 878-886.
[45] Winkelman JW, Johnston L. Augmentation and tolerance with long-term pramipexole treatment of restless legs syndrome (RLS) [J]. Sleep Med, 2004, 5(1): 9-14.
[46] Garcia-Borreguero D, Allen RP, Kohnen R, et al. Diagnostic standards for dopaminergic augmentation of restless legs syndrome: report from a World Association of Sleep Medicine-International Restless Legs Syndrome Study Group consensus conference at the Max Planck Institute [J]. Sleep Med, 2007, 8(5): 520-530.
[47] Hornyak M, Scholz H, Kohnen R, et al. What treatment works best for restless legs syndrome? Meta-analyses of dopaminergic and non-dopaminergic medications [J]. Sleep Med Rev, 2014, 18(2): 153-164.
收稿日期:(2014-06-02)
通訊作者:**金莉蓉,副主任醫(yī)師,主要從事帕金森病等運動障礙的臨床和基礎研究。E-mail: jinlr99@163. com
作者簡介:*喻哲明,住院醫(yī)師,主要從事帕金森病的臨床和基礎研究
文章編號:1006-1533(2015)03-0018-05
文獻標識碼:A
中圖分類號:R971.5; R741.05