PLR和NLR在慢性阻塞性肺疾病急性加重病情評估中的 臨床價值
胡斯明 徐曉 徐國鵬
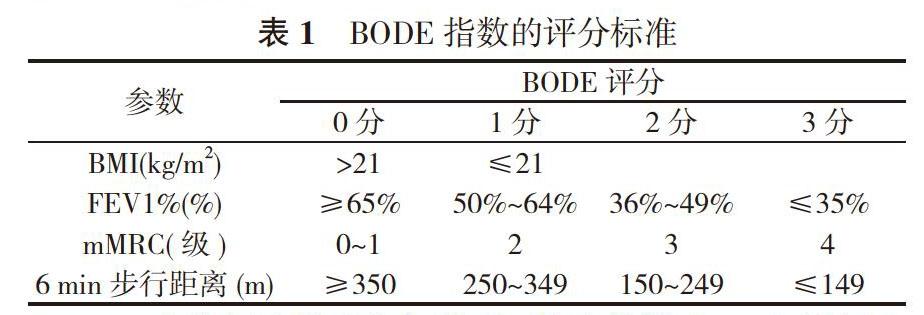
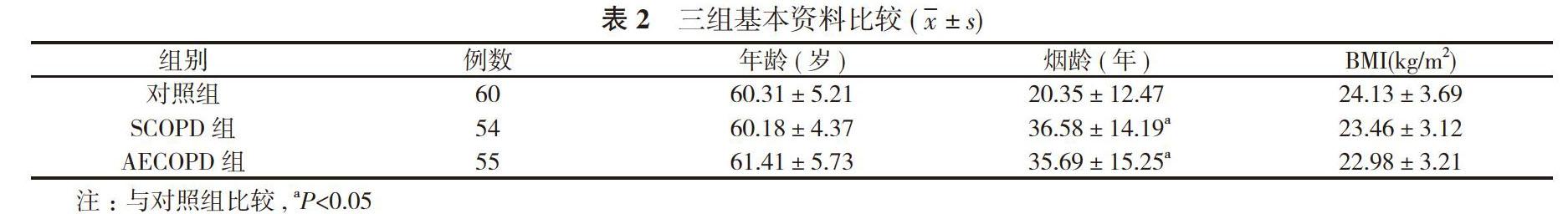
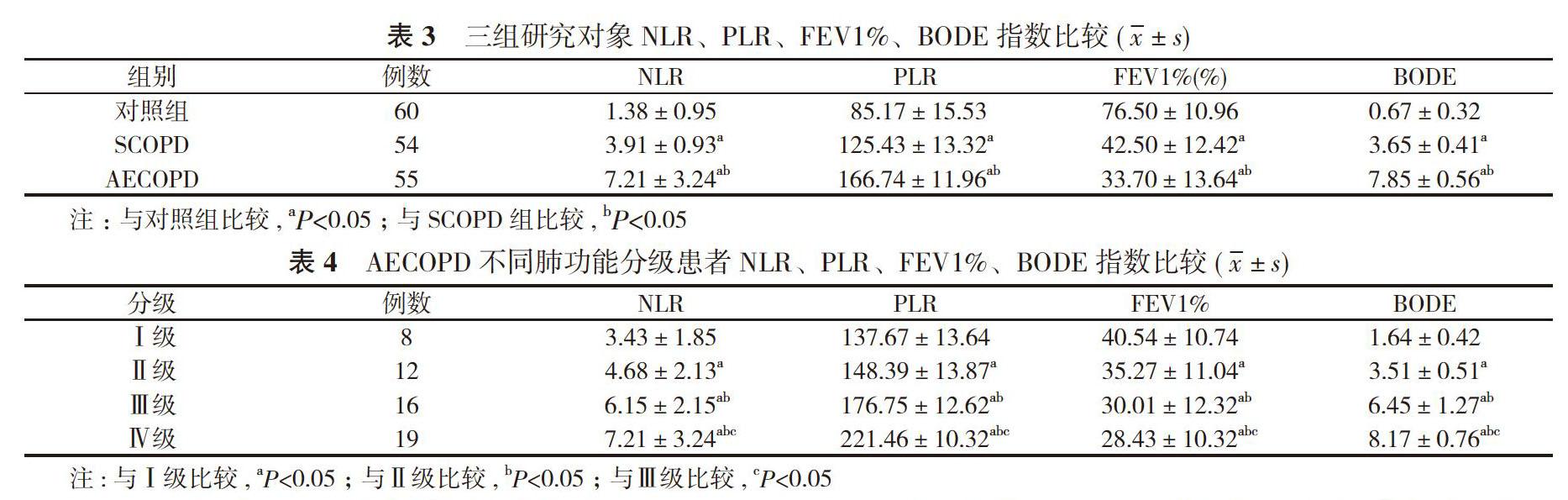
【摘要】 目的 探討中性粒細胞與淋巴細胞比值(NLR)、血小板與淋巴細胞比值(PLR)在慢性阻塞性肺疾病急性加重(AECOPD)病情評估中的臨床價值。方法 選擇55例AECOPD患者作為AECOPD 組, 54例慢性阻塞性肺疾病穩定期(SCOPD)患者作為SCOPD 組, 同期體檢的60例健康體檢者作為對照組。比較三組研究對象基本資料、NLR、PLR、第1秒用力呼氣容量占預計值的百分比(FEV1%)、BODE指數;比較AECOPD不同肺功能分級患者NLR、PLR、FEV1%、BODE指數;分析NLR、PLR與BODE 指數的相關性, NLR、PLR在AECOPD中的診斷效能。結果 對照組煙齡短于SCOPD組、AECOPD組, 差異具有統計學意義(P<0.05);SCOPD組、AECOPD組患者煙齡比較差異無統計學意義(P>0.05)。三組研究對象年齡、體質量指數(BMI)比較差異無統計學意義(P>0.05)。三組研究對象NLR、PLR、FEV1%、BODE指數比較差異具有統計學意義(P<0.05)。AECOPD肺功能分級Ⅰ級8例, Ⅱ級12例, Ⅲ級16例, Ⅳ級19例。AECOPD不同肺功能分級患者NLR、PLR、FEV1%、BODE指數比較差異具有統計學意義(P<0.05), 隨著分級的增加, NLR、PLR、BODE指數增加, FEV1%降低。NLR、PLR與BODE 指數呈正相關(r=0.751、0.748, P<0.05)。NLR的ROC曲線下面積為0.87, 95%CI=(0.139, 0.731), 敏感度為88%, 特異度為86%;PLR的ROC曲線下面積為0.74, 95%CI=(0.614, 0.902), 敏感度為82%, 特異度為80%。
結論 NLR和PLR對AECOPD有較好的診斷效能, 與 BODE 指數具有相關性, 可作為評估慢性阻塞性肺疾病病情及預后的便捷、實用的臨床指標。
【關鍵詞】 慢性阻塞性肺疾病;急性加重;中性粒細胞;淋巴細胞;血小板
DOI:10.14163/j.cnki.11-5547/r.2019.33.003
Clinical value of PLR and NLR in evaluation of disease condition of patients with acute exacerbation of chronic obstructive pulmonary disease ? HU Si-ming, XU Xiao, XU Guo-peng, et al. Department of Respiratory Medicine, Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou 215000, China
【Abstract】 Objective ? To discuss the clinical value of neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR) in evaluation of disease condition of patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Methods ? There were 55 AECOPD patients as AECOPD group, 54 patients with stable-stage chronic obstructive pulmonary disease (SCOPD) as SCOPD group, and 60 healthy people as the control group. The basic data, forced expiratory volume in the first second as percentage of predicted value (FEV1%) and BODE index was compared in three groups, and NLR, PLR, FEV1% and BODE index was compared in patients with different pulmonary function grades of AECOPD. The correlation between NLR, PLR and BODE index, and diagnostic efficiency of NLR and PLR in AECOPD was analyzed. Results ? The smoking time of control group was shorter than those of SCOPD group and AECOPD group, and the difference was statistically significant (P<0.05). There was no statistically significant difference in smoking time between SCOPD group and AECOPD group (P>0.05). There was no statistically significant difference in age and body mass index (BMI) in three groups (P>0.05). There was statistically significant difference in NLR, PLR, FEV1% and BODE index among three groups (P<0.05). The AECOPD pulmonary function classification grade Ⅰ in 8 cases, grade Ⅱ in 12 cases, grade Ⅲ in 16 cases and grade Ⅳ in 19 cases. There were statistically significant differences in NLR, PLR, FEV1% and BODE index among the patients with different pulmonary function grades of AECOPD (P<0.05). With the increase of grades, NLR, PLR, BODE index increased, FEV1% decreased. NLR and PLR were positively correlated with BODE index (r=0.751、0.748, P<0.05). The area under ROC curve of NLR was 0.87, 95%CI=(0.139, 0.731), sensitivity was 88%, specificity was 86%; the area under ROC curve of PLR was 0.74, 95%CI=(0.614, 0.902), sensitivity was 82%, specificity was 80%. Conclusion ?NLR and PLR shows good diagnostic effect on AECOPD, and are correlated with BODE index. They can be used as a convenient and practical clinical index to evaluate the condition and prognosis of COPD.
2. 4 NLR、PLR與BODE 指數相關性分析 NLR、PLR與BODE 指數呈正相關(r=0.751、0.748, P<0.05)。
2. 5 PLR和NLR對AECOPD的診斷效能分析 NLR的ROC曲線下面積為0.87, 95%CI=(0.139, 0.731), 敏感度為88%, 特異度為86%;PLR的ROC曲線下面積為0.74, 95%CI=
(0.614, 0.902), 敏感度為82%, 特異度為80%。見圖1。
3 討論
COPD是一種慢性氣道炎癥性疾病, 具有不完全可逆性氣流受限特征, 是全球范圍內引起慢性疾病死亡的主要疾病之一, 預計到2030年COPD將成為全球第三大致死性疾
病[7]。COPD急性發作將導致患者生存質量明顯下降, 嚴重者出現呼吸衰竭等并發癥, 加速肺功能惡化, 嚴重影響預后, 增加死亡率。因而, 從2011年COPD診斷治療預防全球策略 (global initiative for chronic obstructive lung disease , GOLD)開始將急性加重風險納入對COPD病情的綜合評估中來。因此, 及早發現、干預及預防AECOPD發生對臨床具有重要意義。
大多數AECOPD的誘發因素為感染性因素, 包括細菌、病毒感染等, 炎癥反應對AECOPD的發生、發展起到關鍵作用。通過對COPD患者炎癥狀態的評估可以預防AECOPD發生、評估患者預后。因此與炎癥反應相關的血清標志物如CRP、PCT、IL-6等被應用于AECOPD患者臨床病情評估中。但這些指標均存在一定的優缺點, 如CRP受較多其他因素影響, PCT敏感度較高但不能預測預后, IL-6等炎性介質的監測較復雜、費用高等, 如何尋找客觀、簡便的方法早期診斷、及時評估AECOPD病情嚴重程度及預后成為目前研究的
方向。
近年來發現NLR、PLR做為新的炎癥診斷標志物在各種應激刺激下的炎癥性疾病(如腫瘤、肺炎、急性肺栓塞等)中起到重要的作用[8-10]。研究表明NLR、PLR與多種肺部疾病如肺結核、COPD等有關。Karadeniz等[11]發現COPD患者PLR水平高于健康對照組, AECOPD患者PLR水平明顯高于穩定期。Furutate等[12]發現AECOPD患者NLR水平高于穩定期, 并且NLR水平與肺氣腫程度、mMRC評分呈正相關, 與6 min步行距離呈負相關, 因此認為NLR與COPD嚴重程度及急性發作有關。與之前學者研究結果相同, 本研究發現隨著AECOPD病情的加重, NLR、PLR逐漸增高。本研究根據ROC曲線分析, NLR的ROC曲線下面積為0.87, 敏感度為88%, 特異度為86%。PLR的ROC曲線下面積為0.74, 敏感度為82%, 特異度為80%。分析顯示, NLR、PLR在判斷AECOPD方面有著良好的預測價值, 同時具有較好的敏感度和特異度, 表明NLR、PLR在預測AECOPD及評估嚴重程度方面具有一定的臨床意義。
臨床上評估COPD患者病情的指標有很多, 但因COPD作為一種全身性疾病, 許多指標無法全面系統的反映COPD病情。2004年由Celli等[13]提出BODE指數, 從臨床癥狀、運動能力、肺功能和營養狀態等多方面, 全面評估COPD患者病情, 系統反映COPD患者的呼吸功能和全身效應, 受到廣泛認同。本研究采用相關性分析發現, NLR、PLR與BODE指數均存在顯著相關關系, 說明NLR、PLR在COPD疾病病情評估方面具有重要臨床意義, 聯合檢測可以提高可靠性和敏感度。
綜上所述, 臨床工作中, 在BODE系統基礎上加入PLR、NLR等生物標志物, 進行多因素綜合評定, 可為臨床診治提供方便快捷的評估方法, 降低不良預后風險, 改善疾病預后。然而, 由于本研究受到各種客觀因素等的影響, 對于NLR和PLR在AECOPD和SCOPD患者疾病過程中的病理生理機制還需進一步的研究。
參考文獻
[1] Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary diseas: GOLD executive summary. Am J Res Critical Care Medicine, 2013, 187(4):347-365.
[2] Tomaki M, Sugiura H, Koarai A, et al. Decreased expression of antioxidant enzymes and increased expression of chemokines in COPD lung. Pulm Pharmacol Ther, 2007, 20(5):596-605.
[3] Günay E, Sar?n? Ula?l? S, et al. Neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease: a retrospective study. In?ammation, 2014, 37(2):374-380.
[4] Kurtipek E, Bekci TT, Kesli R, et al. The role of neutrophil-lymphocyte ratio and platelet lymphocyte-ratio in exacerbation of chronic obstructive pulmonary disease. J Pak Med Assoc, 2015, 65(12):1283?1287.
[5] 中華醫學會呼吸病學會慢性阻塞性肺疾病學組. 慢性阻塞性肺疾病診治指南(2013年)修訂版. 中華結核和呼吸雜志, 2013, 36(4):1.
[6] Rahman S. Prognostic Evaluation of COPD Patients using BODE Index. Chest, 2014, 146(4):30A.
[7] Burney PG, Patel J, Newson R, et al. Global and regional trends in COPD mortality, 1990-2010. Eur Respir J, 2015, 45(5):1239-1247.
[8] Azab B, Shah N, Akerman M, et al. Value of platelet/lymphocyte ratio as a predictor of all-cause mortality after non-STelevation myocardial infarction. J Thromb Thrombolysis, 2012, 34(3):326-334.
[9] Yang T, Wan C, Wang H, et al. The prognostic and risk stratifed value of neutrophil-lymphocyte count ratio in Chinese patients with community-acquired pneumonia. Eur J In?amm, 2017, 15(1):22-27.
[10] Karata? MB, ?pek G, Onuk T, et al. Assessment of prognostic value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in patients with pulmonary embolism. Acta Cardiol Sin, 2016, 32(3):313-320.
[11] Karadeniz G, Akto?u S, Erer OF, et al. Predictive value of platelet to lymphocyte ratio in exacerbation of chronic obstructive pulmonary disease. Biomarkers, 2016, 10(7):701?710.
[12] Furutate R, Ishii T, Motegi T, et al. The neutrophil to lymphocyte ratio is related to disease severity and exacerbation in patients with chronic obstructive pulmonary disease. Intern Med, 2016, 55(3): 223?229.
[13] Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med, 2004, 350(10):1005-1012.
[收稿日期:2019-07-02]