前置胎盤(pán)產(chǎn)婦合并胎盤(pán)植入危險(xiǎn)因素及對(duì)產(chǎn)婦與新生兒的影響
曹殿玲
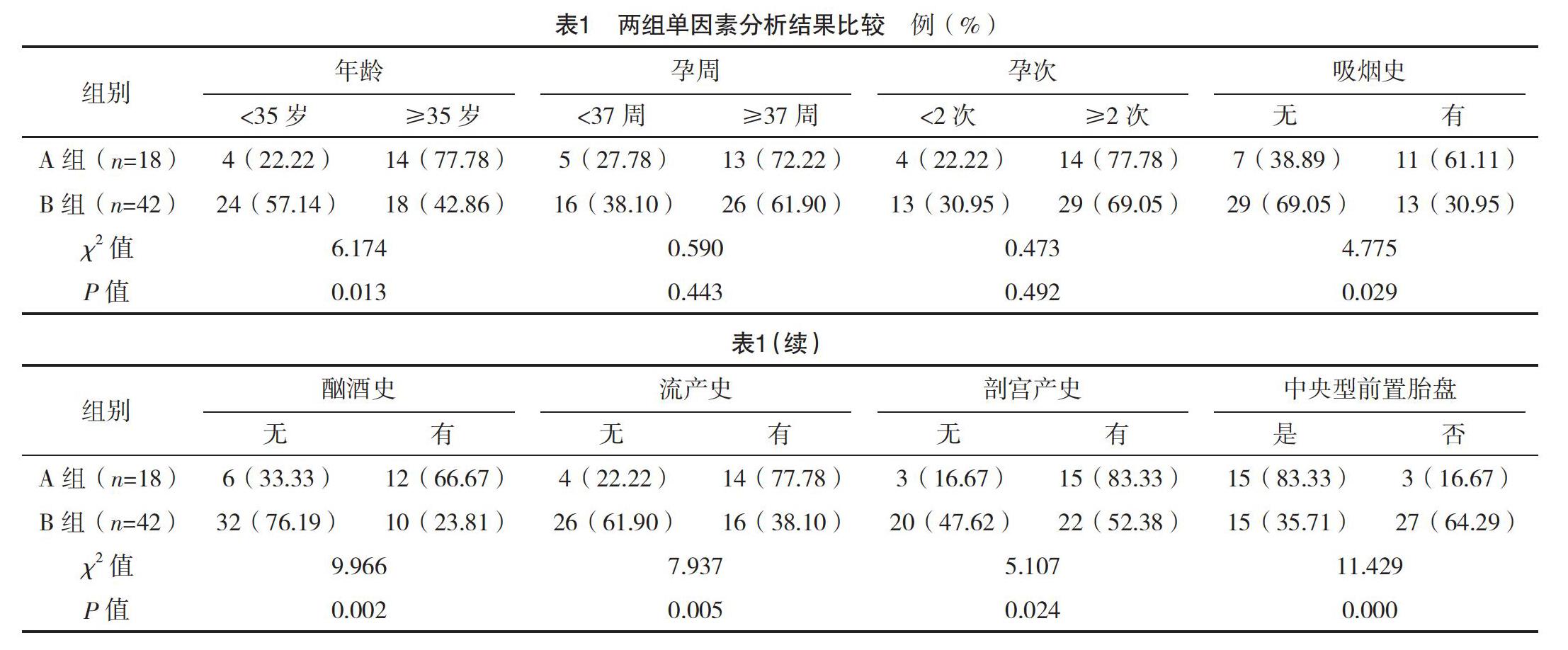
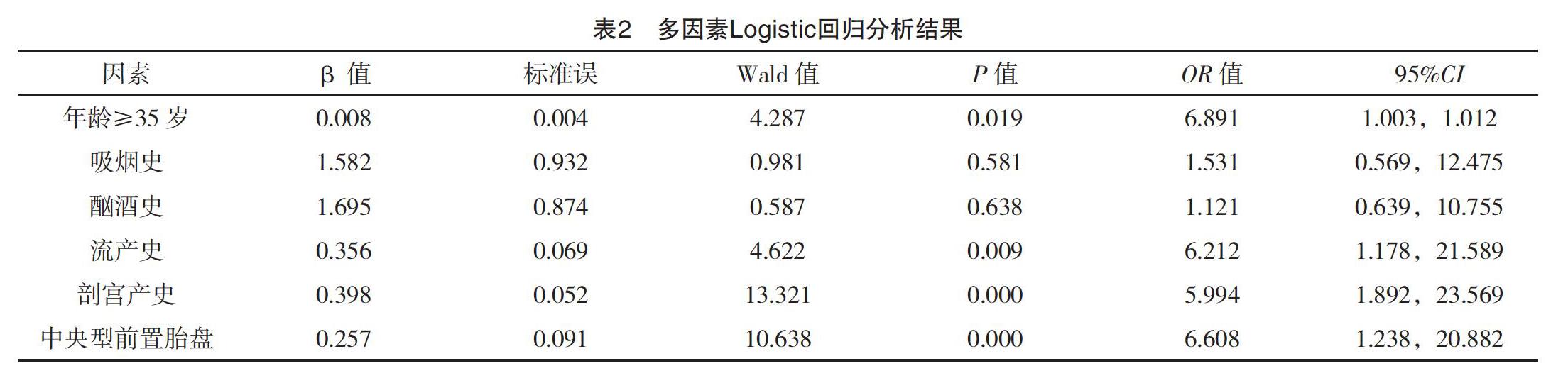
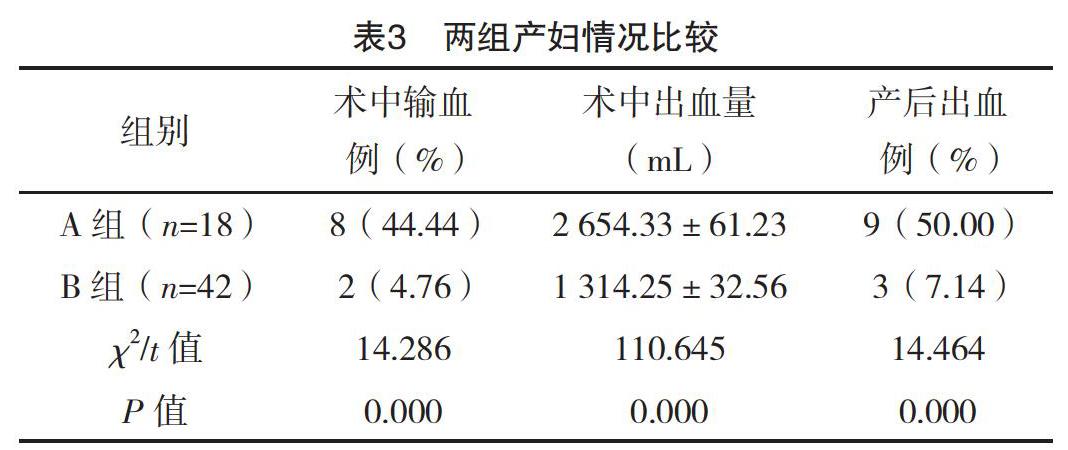
【摘要】 目的:分析前置胎盤(pán)產(chǎn)婦合并胎盤(pán)植入危險(xiǎn)因素及對(duì)產(chǎn)婦與新生兒的影響。方法:選取本院2015年1月-2018年11月產(chǎn)科收治的60例前置胎盤(pán)產(chǎn)婦作為觀察對(duì)象,對(duì)其臨床資料進(jìn)行回顧性分析。對(duì)所有產(chǎn)婦年齡、吸煙史、酗酒史、流產(chǎn)史、剖宮產(chǎn)史、前置胎盤(pán)類(lèi)型等進(jìn)行分析。根據(jù)是否合并胎盤(pán)植入分為A、B組,A組(n=18)發(fā)生胎盤(pán)植入,B組(n=42)未發(fā)生胎盤(pán)植入。對(duì)兩組產(chǎn)婦情況及新生兒情況進(jìn)行分析。結(jié)果:兩組年齡、吸煙史、酗酒史、流產(chǎn)史、剖宮產(chǎn)史及前置胎盤(pán)類(lèi)型比較,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05),但兩組孕周、孕次比較,差異均無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05)。多因素分析結(jié)果顯示,年齡≥35歲、流產(chǎn)史、剖宮產(chǎn)史及中央性前置胎盤(pán)是合并胎盤(pán)植入的獨(dú)立危險(xiǎn)因素(P<0.05);A組產(chǎn)婦術(shù)中輸血率、產(chǎn)后出血率及術(shù)中出血量均高于B組,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05);A組新生兒窒息率(44.44%)與早產(chǎn)率(27.78%)均高于B組的4.76%、0,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05)。A組新生兒1 min Apgar評(píng)分(7.02±0.42)分、出生體重(3.07±0.47)kg均低于B組的(8.32±0.88)分、(3.99±0.89)kg,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05)。結(jié)論:前置胎盤(pán)嚴(yán)重威脅產(chǎn)婦及新生兒安全,合并胎盤(pán)植入與年齡、流產(chǎn)史、剖宮產(chǎn)史、中央性前置胎盤(pán)存在密切的關(guān)聯(lián),合并胎盤(pán)植入后,產(chǎn)婦和新生兒風(fēng)險(xiǎn)均明顯增加。
【關(guān)鍵詞】 前置胎盤(pán) 胎盤(pán)植入 危險(xiǎn)因素
[Abstract] Objective: To analyze the risk factors of placenta previa combined with placental implantation and its influence on the pregnant women and newborns. Method: The clinical data of 60 pregnant women with placenta previa admitted to the obstetrics department of our hospital, from January 2015 to November 2018 were retrospectively analyzed. The age, smoking history, alcoholism history, abortion history, cesarean section history and type of placenta previa were analyzed. According to the combination of placental implantation or not, they were divided into group A and B. Placental implantation occurred in group A (n=18) and no placental implantation occurred in group B (n=42). The parturient and neonatal condition of two groups were analyzed. Result: There were significant differences in age, smoking history, alcohol abuse history, abortion history, cesarean section history and placenta previa type between the two groups (P<0.05). However, there were no statistically significant differences in gestational weeks and gestational times between the two groups (P>0.05). Multivariate analysis showed that age≥35 years, history of abortion, cesarean section and central placenta previa were independent risk factors for placental implantation (P<0.05). The intraoperative blood transfusion rate, postpartum hemorrhage rate and intraoperative hemorrhage volume in group A were higher than those in group B, the differences were statistically significant(P<0.05). The neonatal asphyxia rate (44.44%) and premature delivery rate (27.78%) in group A were higher than 4.76%, 0 in group B, the differences were statistically significant(P<0.05). The 1 min Apgar score (7.02±0.42) scores and birth weight (3.07±0.47) kg in group A were lower than (8.32±0.88) scores, (3.99±0.89) kg in group B, the differences were statistically significant(P<0.05). Conclusion: Placenta previa is a serious threat to maternal and neonatal safety, placenta previa combined with placenta implantation is closely related to age, abortion history, cesarean section history and central placenta previa, after placenta implantation, maternal and neonatal risks increase significantly.
[2]曾義,李杰,段光友,等.再次剖宮產(chǎn)產(chǎn)后出血危險(xiǎn)因素分析:2442例產(chǎn)婦的回顧性研究[J].第三軍醫(yī)大學(xué)學(xué)報(bào),2019,41(3):265-269.
[3]劉芳,羅瑋.伴瘢痕子宮的前置胎盤(pán)產(chǎn)婦手術(shù)情況及新生兒結(jié)局觀察[J].中外醫(yī)學(xué)研究,2018,16(32):8-10.
[4]黨志霞.胎盤(pán)植入產(chǎn)婦相關(guān)危險(xiǎn)因素及結(jié)局分析[J].中外醫(yī)療,2018,37(31):43-45.
[5]蔡本碩,杜鵑.某醫(yī)院前置胎盤(pán)患者術(shù)中出血相關(guān)因素的回顧性分析[J].東南大學(xué)學(xué)報(bào)(醫(yī)學(xué)版),2018,37(5):908-911.
[6]吳爭(zhēng)勇,劉麗群.彩超診斷中央性前置胎盤(pán)并胎盤(pán)植入的臨床分析[J].現(xiàn)代診斷與治療,2018,29(20):3253-3254.
[7]陳陶玲,李銀華,張小英.產(chǎn)前超聲檢查在前置胎盤(pán)及植入孕婦分娩大出血預(yù)測(cè)中的臨床應(yīng)用價(jià)值[J/OL].心電圖雜志(電子版),2018,7(3):27-30.
[8]楊凱樂(lè),劉展,謝菲,等.前置胎盤(pán)并胎盤(pán)植入的高危因素及對(duì)妊娠結(jié)局的影響[J].實(shí)用預(yù)防醫(yī)學(xué),2018,25(9):1105-1107.
[9]郭吉敏,曹滿(mǎn)瑞,劉小平,等.MRI征象回歸模型在植入型兇險(xiǎn)性前置胎盤(pán)的應(yīng)用[J].臨床放射學(xué)雜志,2018,37(8):1325-1328.
[10]劉冬紅,李華麗,李維玲.前置胎盤(pán)伴胎盤(pán)植入術(shù)中應(yīng)用宮頸COOK雙球囊及卡前列素氨丁三醇防治產(chǎn)后出血療效觀察[J].中國(guó)計(jì)劃生育學(xué)雜志,2018,26(8):731-733.
[11]覃獻(xiàn)珍.導(dǎo)致中央型前置胎盤(pán)剖宮產(chǎn)后出血的危險(xiǎn)因素分析[J].世界最新醫(yī)學(xué)信息文摘,2018,18(66):35.
[12] Karami M,Jenabi E,F(xiàn)ereidooni B.The association of placenta previa and assisted reproductive techniques:a meta-analysis[J].The Journal of Maternal-Fetal & Neonatal Medicine,2017:1-18.
[13]薛曉玲.前置胎盤(pán)合并剖宮產(chǎn)史患者產(chǎn)后大出血危險(xiǎn)因素研究[J].中外女性健康研究,2018(12):84,87.
[14]邱文山,黎法文,林小蘭,等.90例兇險(xiǎn)性前置胎盤(pán)的回顧性研究及危險(xiǎn)因素分析[J].廣東醫(yī)科大學(xué)學(xué)報(bào),2018,36(2):211-213.
[15]李玉梅,楊文才,陳健聰,等.一站式球囊封堵術(shù)輔助中央性前置胎盤(pán)剖宮產(chǎn)術(shù)的護(hù)理路徑管理[J].實(shí)用醫(yī)院臨床雜志,2018,15(3):125-127.
[16]王恒宇,何明祥,漆洪波.兇險(xiǎn)性前置胎盤(pán)腹主動(dòng)脈球囊阻斷下剖宮產(chǎn)術(shù)子宮切除的相關(guān)影響因素及母嬰結(jié)局研究[J].醫(yī)學(xué)信息,2018,31(8):49-52.
[17]張力維,李青,齊淑琴,等.前置胎盤(pán)伴胎盤(pán)植入危險(xiǎn)因素分析及宮頸子宮下段環(huán)形縫合術(shù)對(duì)母嬰結(jié)局的影響[J].中國(guó)現(xiàn)代醫(yī)生,2018,56(6):56-59.
[18] Feng Y,Li X Y,Xiao J,et al.Risk Factors and Pregnancy Outcomes:Complete versus Incomplete Placenta Previa in Mid-pregnancy[J].Current Medical Science,2018,38(4):597-601.
[19]連旭波,韋春杏.妊娠期兇險(xiǎn)型前置胎盤(pán)的核磁共振成像診斷價(jià)值與妊娠結(jié)局的關(guān)系[J].中國(guó)計(jì)劃生育和婦產(chǎn)科,2018,10(1):28-31.
[20]石巍.子宮破裂及前置胎盤(pán)與瘢痕子宮再妊娠患者剖宮產(chǎn)產(chǎn)后出血的關(guān)聯(lián)性分析[J].內(nèi)蒙古醫(yī)學(xué)雜志,2017,49(12):1436-1438.
[21]李娟,付金紅,張慧娟,等.兇險(xiǎn)性前置胎盤(pán)植入原因及母嬰結(jié)局的影響回顧性研究[J].河北醫(yī)藥,2017,39(23):3575-3578.
[22]王志英.前置胎盤(pán)導(dǎo)致選擇性剖宮產(chǎn)產(chǎn)婦大出血的影響因素研究[J].中外女性健康研究,2018(12):73-75.
[23]董南,胥琪琪,葉敏清,等.兇險(xiǎn)型前置胎盤(pán)狀態(tài)伴胎盤(pán)植入中期妊娠引產(chǎn)一例[J/OL].中華產(chǎn)科急救電子雜志,2018,7(1):54-57.
(收稿日期:2019-06-10) (本文編輯:田婧)
 中國(guó)醫(yī)學(xué)創(chuàng)新2019年32期
中國(guó)醫(yī)學(xué)創(chuàng)新2019年32期
- 中國(guó)醫(yī)學(xué)創(chuàng)新的其它文章
- 右美托咪定復(fù)合地佐辛對(duì)腹腔鏡膽囊切除患者鎮(zhèn)痛的效果及對(duì)血漿兒茶酚胺、ET-1的影響
- 雙心護(hù)理模式在急診PCI治療急性心肌梗死護(hù)理中的應(yīng)用及對(duì)患者預(yù)后的影響
- Chest:COPD-OSA重疊綜合征診治進(jìn)展
- 1.5T磁共振在卵巢囊腺瘤臨床診斷中的應(yīng)用及其影像特點(diǎn)分析
- 腹部手術(shù)后患者急性應(yīng)激障礙及其相關(guān)影響因素的研究
- 探討LncRNA遺傳多態(tài)性及其與結(jié)直腸癌風(fēng)險(xiǎn)和預(yù)后的相關(guān)性
