預測評分量表對卒中相關性肺炎的應用價值
舒兆瑞 王兵 張克飛
摘要:目的? 分析多種卒中相關性肺炎危險因素預測評分表的特點及其臨床應用價值。方法? 檢索PubMed和CNKI中有關卒中相關性肺炎危險因素預測評分表的文獻,包括針對SAP制定預測評分表的文獻及應用現有卒中相關評分表預測SAP的文獻,用診斷試驗質量評價工具(QUADAS-2)對文獻報道的預測評分量表進行危險因素評分,分析相關評分與卒中相關性肺炎診斷率的關系,評估相關預測評分的臨床應用價值。結果? 共檢索到238篇相關研究文獻,針對SAP制定預測評分表的文獻162篇,應用現有卒中相關評分表預測SAP的文獻76篇,共涉及13種預測評分表,其中年齡和NIHSS評分幾乎在所有預測評分表中都有出現。對6種評分表進行了內部驗證,5種評分表進行了外部驗證,A2DS2評分是目前最受認可的,其敏感性和特異性均高于其他預測評分表。結論? 臨床預測模型在應用時簡單易行,不同評分表之間的敏感性和特異性是相似的。目前預測評分表對卒中相關性肺炎有一定的應用價值,但缺乏相關大型研究評價這些評分表對臨床決策和預后的影響,其實用性仍需更多的臨床研究來驗證。
關鍵詞:卒中相關性肺炎;預測評分量表;危險因素;年齡;NIHSS評分
中圖分類號:R743.3? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? 文獻標識碼:A? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? DOI:10.3969/j.issn.1006-1959.2020.01.038
文章編號:1006-1959(2020)01-0124-03
Application Value of Predictive Scoring Scale for Stroke-associated Pneumonia
SHU Zhao-rui,WANG Bing,ZHANG Ke-fei
(Department of Neurology,Huai'an Hospital,Nanjing University of Traditional Chinese Medicine,Huai'an 223001,Jiangsu,China)
Abstract:Objective To analyze the characteristics of multiple stroke-associated pneumonia risk factor prediction scores and their clinical application value. Methods? Retrieve the relevant literature on the risk-related predictive scores for stroke-associated pneumonia in PubMed and CNKI, including the literature on the development of predictive scores for SAP and the literature on the use of existing stroke-related scores to predict SAP.The diagnostic test quality assessment tool (QUADAS-2) was used to evaluate the risk factor scores of the predictive score scales reported in the literature, and the relationship between the relevant scores and the diagnosis rate of stroke-associated pneumonia was analyzed to evaluate the clinical application value of the relevant predictive scores.Results? A total of 238 related research literatures were retrieved, 162 were used to develop predictive scores for SAP, and 76 were used to predict SAP using existing stroke-related scores. A total of 13 predictive scores were involved, including age and NIHSS scores in almost all all appear in the forecast score sheet. 6 types of scoring tables were verified internally and 5 types of scoring tables were externally verified. The A2DS2 score is currently the most recognized, and its sensitivity and specificity are higher than other predictive score tables.Conclusion? The clinical prediction model is simple and easy to apply, and the sensitivity and specificity are similar among different scoring tables. At present, the predictive scores have certain application value for stroke-related pneumonia, but there is a lack of large-scale studies to evaluate the impact of these scores on clinical decision-making and prognosis, and its practicality needs to be verified by more clinical studies.
Key words:Stroke-associated pneumonia;Predictive scoring scale;Risk factors;Age;NIHSS score
自Hilker R等[1]2003年提出卒中相關性肺炎(SAP)的概念后,臨床上對該病的診治在不斷探索中取得了較大的進展,卒中相關性肺炎診斷專家共識[2]建議將卒中急性期并發的一系列下呼吸道感染統稱為SAP,并將SAP的發病時間限定為卒中發病后7 d內,進一步明確了該病的診斷標準。為早期預測SAP的發生風險,針對該病的預測模型也在不斷研究中,但目前仍缺乏高質量的循證醫學證據,相關模型量表的建立不僅可以對SAP風險進行評估,也可以為相應治療療效的評定提供參考。本文主要對近年來SAP預測模型相關量表進行對比,以期為建立更有價值的預測模型提供參考依據。
1資料與方法
1.1數據來源? 在PubMed和CNKI進行中,使用關鍵詞肺炎、腦梗死、腦出血、腦卒中、危險評分、卒中相關性肺炎進行自動檢索,檢索時間設定為2003年1月~2019年5月。同時手動檢索一些潛在的可能符合條件的文章。
1.2數據篩選和分組? 檢索目前已應用于臨床、且有相關文獻報道的預測評分模型(按時間先后順序)并分組:組1:針對SAP制定預測評分表的文獻;組2:應用現有卒中相關評分表預測SAP的文獻。檢索到的文獻必須具備條件:相關研究文獻應用Logistic回歸模型分析SAP的獨立危險因素,統計獨立危險因素制定表。
1.3數據統計分析? 分析檢索到的評分表的組成、樣本數量、內部驗證、外部驗證、特異性和敏感性,使用診斷試驗質量評價工具(QUADAS-2)對評分表進行適用性和風險性評估,由兩人分別獨立完成評估。比較各個預測評分表的靈敏度和特異度,用Youde指數確定最佳診斷界值,檢驗水準α=0.05,P<0.05表示差異有統計學意義。
2結果
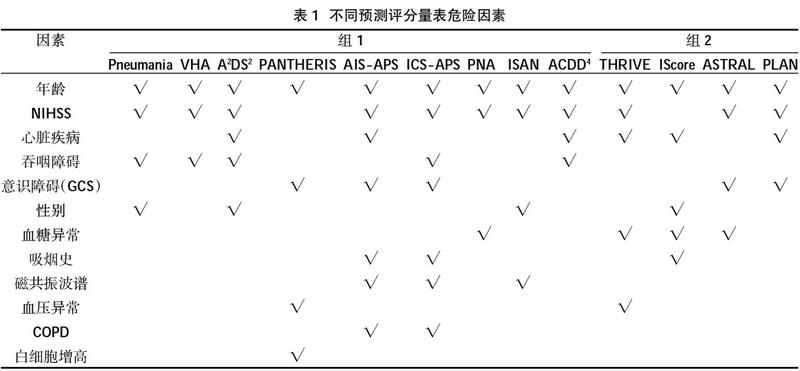
2.1檢索情況? 共檢索到238篇相關研究文獻,組1和組2分別為162篇、76篇,共涉及13種量表。組1中量表包括:The Pneumania Score[3]、VHA Score(Veteran's Health Administration Cohort Score)[4]、A2DS2[5]、PANTHERIS[6]、AIS-APS[7]、ICS-APS[8](ICS-APS-A;ICS-APS-B)、PNA(Pneumonia)Score[9]、ISAN (Prestroke Independence,Sex,Age,NIHSS)Score[10]及ACDD4[11]。組2中量表包括THRIVE Score[12]、IScore[13]、ASTRAL[14]、PLAN Score(Preadmission Comorbidities,Level of Consciousness,Age,Neurologic Deficit)[15]。其中年齡是每個預測評分量表都有的項目,NIHSS評分除PANTHERIS和IScore Score中沒有外,其他預測評分表也都有。但IScore Score應用了CNS評分評估卒中嚴重程度,并且依據需要可相互轉換。不同研究的Logistic回歸模型結果均提示:心臟疾病(房顫、充血性心力衰竭)、吞咽障礙、意識障礙、性別、血糖異常、吸煙史、波譜成像、血壓異常、COPD、白細胞增高可能為SAP的獨立危險因素。但由于NIHSS評分與吞咽障礙、卒中類型、意識障礙均有較強的相關性,可能導致多因素Logistic回歸部分結果偏差甚至無法解釋,故部分研究在統計時未將NIHSS評分納入多因素Logistic模型中。13種預測評分量表涉及的因素見表1。
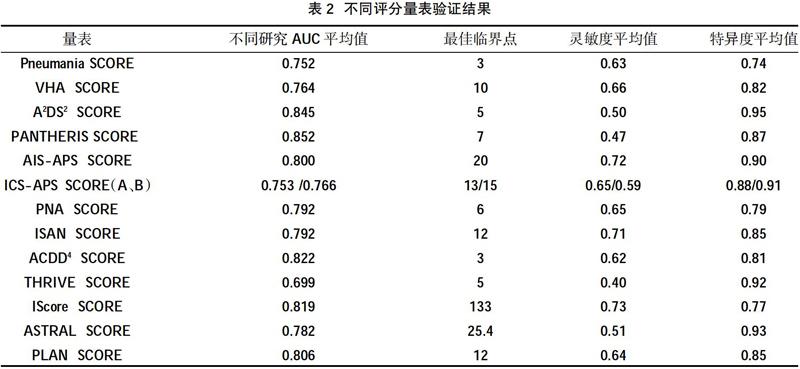
2.2風險評分驗證結果? 分別統計不同量表的Youden指數并選擇最大切點為臨界點,即(靈敏度+特異度-1)達到最大所對應的值為SAP最佳診斷臨界點,見表2。
3討論
SAP本身的復雜性為臨床診療帶來了諸多困難,該病涉及的危險因素眾多,針對患者不同病理生理階段選擇最佳的預防措施尤為重要,因此準確評估患者病情程度成為臨床研究的重點。本次調查發現,目前臨床中存在較多的SAP危險因素預測評分表,其中年齡和NIHSS評分在大部分量表中都有出現。不同研究的Logistic回歸模型結果均提示:心臟疾病(房顫、充血性心力衰竭)、吞咽障礙、意識障礙、性別、血糖異常、吸煙史、波譜成像、血壓異常、COPD、白細胞增高可能為SAP的獨立危險因素。再一次驗證了年齡、NIHSS、意識障礙、吞咽困難、心臟疾病可能為SAP獨立危險因素。本次研究顯示,A2DS2量表評分≥5分預測SAP的敏感性和特異性分別為95.00%和50.00%,A2DS2的評分項目較少,且均為患者臨床資料,在計算NIHSS評分的前提下較易計算,臨床操作性較強。同時,在現有的卒中預測量表中,ASTRAL SCORE量表也表現出較高的準確性。
結合本研究發現,所有文獻報道都詳細記錄了研究樣本的選擇,除了一項前瞻性研究,其他都為回顧性評價。預測評分量表的定義和組成風險因素的方案是多種多樣的,而且常受到數據可用性的限制。如:吞咽困難并不是在所有預測評分量表中都出現,并且卒中前功能障礙評估中就有該項目,只是描述方法不同。還有一些研究并沒有記錄患者入院前已經存在的殘疾。在SAP診斷意見統一之前,各研究的診斷仍存在一定差異[16,17]。目前對于卒中相關性肺炎的診斷率仍偏低,本研究尚需要進一步隨機對照臨床研究以驗證相關SAP獨立危險因素,以制定符合本地區人群發病特點的相應評估量表,以提高對SAP的診斷率,早起預防治療。
綜上所述,SAP危險因素預測評分表使用簡單易行,相應的計分數據也較容易獲得,且在相應的研究中已經證實擁有不錯的預測能力。這些量表不但可以協助臨床醫師提高對SAP的預測評估,制定出相應的治療方案,還可以在患者家屬咨詢有關預后問題時幫助醫患之間溝通。同時今后將進行前瞻性隨機對照研究以驗證相關SAP獨立危險因素,制定符合本地區人群發病特點的相應評估量表,以提高對SAP的診斷率,早起預防治療。
參考文獻:
[1]Hilker R,Poetter C,Findeisen N,et al.Nosocomial pneumonia after acute stroke: implications for neurological intensive care medicine[J].Strok,2003,34(4):975-981.
[2]Smith CJ,Kishore AK,Vail A,et al.Diagnosis of Stroke-Associated Pneumonia Recommendations From the Pneumonia in Stroke Consensus Group[J].Stroke,2015,46(8):2335-2340.
[3]Kwon HM,Jeong SW,Lee SH,et al.The pneumonia score:a simple grading scale for prediction of pneumonia after acute stroke[J].Am J Infect Control,2006,34(2):64-68.
[4]Chumbler NR,Williams LS,Wells CK,et al.Derivation and validation of a clinical system for predicting pneumonia in acute stroke[J].Neuroepidemiology,2010,34(4):193-199.
[5]Hoffmann S,Malzahn U,Harms H,et al.Development of a clinical score (A2DS2) to predict pneumonia in a-cute ischemic stroke[J].Stroke,2012,43(10):2617-2623.
[6]Harms H,Grittner U,Dr?觟ge H,et al.Predicting post-stroke pneumonia:the PANTHERIS score[J].Acta Neurol Scand,2013,128( 3):178-184.
[7]Ji R,Shen H,Pan Y,et al.Novel risk score to predict pneumonia after acute ischemic stroke[J].Stroke,2013,44(5):1303-1309.
[8]Ji R,Shen H,Pan Y,et al.Risk score to predict hospital-acquired pneumonia after spontaneous intracerebral haemorrhage[J],Stroke,2014,45(9):2620-2628.
[9]Friedant AJ,Gouse BM,Boehme AK,et al.A simple prediction score for developing a hospital-acquired infection after acute ischaemic stroke[J].J Stroke Cerebrovasc Dis,2015,24(3):680-686.
[10]Smith CJ,Bray BD,Hoffman A,et al.Can a novel clinical risk score improve pneumonia prediction in acute stroke care? A UK multicenter cohort study[J].J Am Heart Assoc,2015,4(1):1-9.
[11]Kumar S,Marchina S,Massaro J,et al.ACDD4 score:A simple tool for assessing risk of pneumonia after stroke[J].Journal of the Neurological Sciences,2017(372):399-402.
[12]Flint AC,Cullen SP,Faigeles BS,et al.Predicting long-termoutcome after endovascular stroke treatment:the totaled health risks in vascular events score[J].AJNR Am J Neuroradiol,2010,31(7):1192-1196.
[13]Saposnik G,Kapral MK,Liu Y,et al.IScore:a risk score to predict death early after hospitalization for an acute ischemic stroke[J].Circulation,2011,123(7):739-749.
[14]Ntaios G,Faouzi M,Ferrari J,et al.An integer-based score to predict functional outcome in acute ischemic stroke:the ASTRAL score[J].Neurology,2012,78(24):1916-1922.
[15]O'Donnell MJ,Fang J,D'Uva C,et al.The PLAN Score[J].Archives of Internal Medicine,2012,172(20):1548-1556.
[16]De Long ER,De Long DM,Clarke-Pearson DL.Comparing the areas under two or more correlated receiver operating characteristic curves:anonparametric approach[J].Biometrics,1988,44(3):837-845.
[17]Smith CJ,Kishore AK,Vail A.Diagnosis of Stroke-Associated Pneumonia:Recommendations From the Pneumonia in Stroke Consensus Group[J].Stroke,2015,8(46):2335-2340.
收稿日期:2019-09-22;修回日期:2019-10-29
編輯/王朵梅